Ethics for Texas Licensed Professional Counselors (6 hours)
NOTICE: BE SURE TO CLICK THE ARROW AT THE END OF THE TEXT TO RECEIVE CREDIT FOR PART ONE. AFTER YOU COMPLETE PART ONE (TEXT) AND PART TWO (QUIZ) YOU CAN PRINT YOUR CERTIFICATE.
Updates were made to this course on November 20, 2025.
Information about this course:
There are often important changes to rules that govern Texas LPCs. The Texas Behavioral Health Executive Council/Texas State Board of Examiners of Professional Counselors site has a new look that licensees may want to become familiar. We try to make this course as current as possible, but please take the initiative to stay current regarding on-going changes where both adopted changes, as well as proposed changes, to the Texas Administrative Code are listed.
This is an online course for Texas LPCs that allows participants to print their certificates immediately after completion of the online quiz at the end of the course. This six-hour ethics course is a review of the “Consolidated Rulebook for Professional Counseling” published by the Texas Behavioral Health Executive Council and Texas State Board of Examiners of Professional Counselors. This Rule booklet lists the Texas Administrative Code rules applicable to Texas LPCs and is updated frequently to reflect changes in legislative statutes. In 2025, Rulebooks were published in March, July, and November.
The Purpose of This Course:
The purpose of this course is to help Texas LPCs review ethical standards pertinent to the practice of counseling. The course will focus specifically on the statutes and rules codified in the Texas Administrative Code relevant to Texas LPCs and published in the Consolidated Rulebook for Professional Counseling.
Learning Objectives:
Participants will:
1. Identify regulated activities of Texas LPCs found in the Texas Administrative Code, Chapter 681, Subchapter B (Rules of Practice).
2. Identify the authorized counseling methods, techniques and modalities listed in Section 681.31 and the process for determining a licensee’s competence to use a specific approach.
3. Review the different rules identified in Sections 681.35 through 681.38 as they pertain to informed consent, client records, billing and financial arrangements, and conflicts, boundaries, dual relationships, and termination of relationships.
4. Summarize the definition and actions that constitute general ethical requirements in Rule 681.41 and sexual misconduct in Rule 681.42.
5. Identify rules regarding testing, drug and alcohol use, confidentiality and required reporting.
6. Describe rules related to licensees and the council, assumed names, advertising and announcements, research and publications found in Rules 681.46 through 681.50.
Before starting this course, we recommend you review the continuing education requirements for Texas LPCs found at the TSBEPC website.
ETHICS FOR TEXAS LICENSED PROFESSIONAL COUNSELORS (6 HOURS)
Note: One of the best resources for Texas LPCs to stay up-to-date with ethical standards is through the website of the BHEC and Texas State Board of Examiners of Professional Counselors. Many links directly and indirectly related to ethics are found at the site with the option of email notification of updates being sent to licensees.
The Consolidated Rulebook for Professional Counseling was last published by the BHEC on November 14th, 2025. This booklet is published as a courtesy to the public. The website cautions: "You are cautioned against relying solely upon these rulebooks and urged to review the current rules which are available through the links below. Moreover, if a conflict exists between a rulebook and the rules published on the Secretary of State’s website, the version on the Secretary of State’s website shall control. Compliance with the law cannot be excused due to an outdated, mistaken, or erroneous reference in a rulebook."
Keep in mind that, although the latest Rules (published November 14th, 2025) regarding the content of this ethics course (Subchapter B: Rules of Practice) were unchanged since the last Rulebook was published in July, one of the recent key changes not in the "Rules of Practice" section was Rule 681.140 "Requirements for Continuing Education" that went into effect July 20,2025. This change impacts the kinds of courses licensees can take to fulfill continuing education requirements stated in 681.140 (a)(1). The course offered at this site (LPCrenewal.com) was changed from "Improving Cultural Competence for Texas LPCs" to "Competent Care to Three Distinct Populations: African-Americans, Asian-Americans, and Hispanic-Americans" to comply with the new requirements. There are many distinct populations that would be covered by the new Rule and the course offered at this site is in no way the only distinct populations that 681.140 addresses.
Another important change involves reporting of continuing education hours. According to the BHEC website: "Beginning January 1, 2026, all licensees must use CE Broker to track and report continuing education (CE) hours. Licensees will need to create an account and report continuing education before renewing their license." For more information about this requirement from the BHEC/Texas State Board of Examiners of Professional Counselors website, click here.
Most recent Consolidated Rulebook for LPCs. Click the picture below to see Rulebook.
INTRODUCTION:
There are currently over 25,000 active Licensed Professional Counselors in Texas. There are an additional 5,000 LPC Associates. Of this number, a small percentage of licensees will be cited for an ethics violation annually, but the total number of violations is not insignificant.
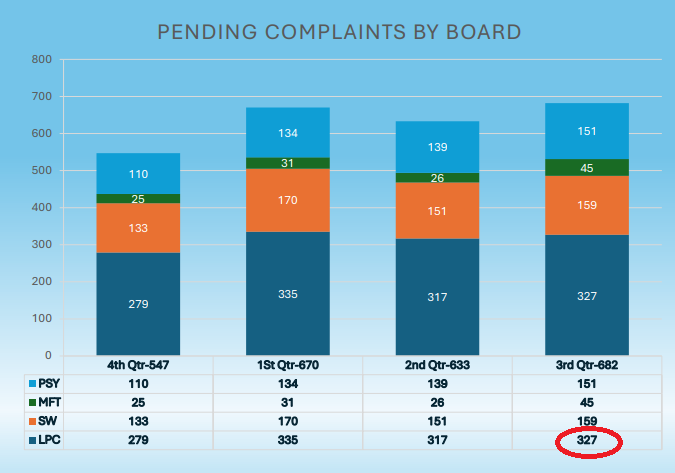
According to the BHEC Enforcement Status Report given at the Full Board Meeting of the TEXAS STATE BOARD OF EXAMINERS OF PROFESSIONAL COUNSELORS held on September 19, 2025, there were 279 total complaints pending against LPCs in Q4 of FY24. This number had increased to 327 by the third quarter of 2025.
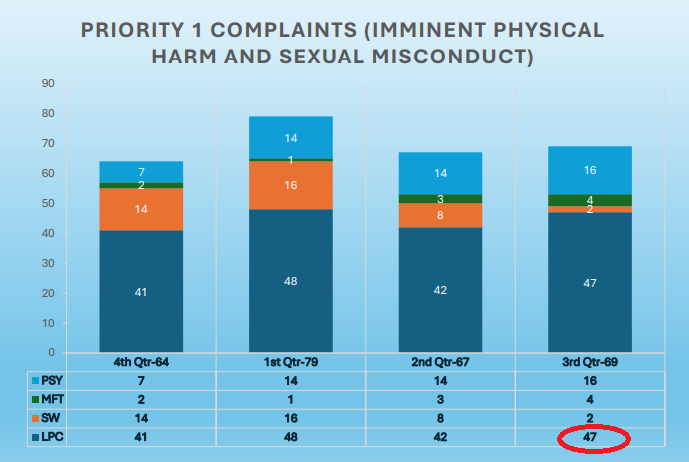
Almost 15% (41 out of 279) of the complaints in Q4 of 2024 involved imminent physical harm and sexual misconduct. The number of complaints in Q3 of 2025 had slightly increased to 47 representing 14% (47 out of 327) of total complaints.
Investigations can be lengthy and time-consuming for both licensees and BHEC staff. Although many complaints are dismissed or involve administrative penalties in the form of a fine, a serious violation has the potential to harm the welfare of a client, impact a community, damage the reputation of the profession, and result in loss of license by the licensee.
Many ethics standards seem to be common sense, while others are unlikely to be known intuitively and their application require careful study. Rules governing LPCs frequently change and can have significant conequences for those unfamiliar with the changes. For instance, the jurisprudence exam was previously a one-tme requirement, but is now required every renewal period for Texas LPCs. Staying informed and current can prevent problems with license renewal and an ethics violation. Fines related to failure to complete continuing education requirements has often been one of the most common infractions for licensees.
Knowledge of any particular ethics code does not guarantee ethical decision-making, but it is a starting point in the aim to prevent harm to the public. This course hopes to remind licensees of some of the obvious, and not-so obvious, ethical obligations Texas LPCs must fulfill.
Texas Statutory framework: Texas Administrative Code
The Texas Administrative Code (TAC) is a compilation of all state agency rules in Texas. Each title represents a subject category and related agencies are assigned to the appropriate title. The Texas Secretary of State compiles and maintains the Code. However, the Secretary of State does not interpret or enforce it. The rules applicable to Texas Licensed Professional Counselors are enforced by the Texas Behavioral Health Executive Council (BHEC) which adopts rules recommended by the Texas State Board of Examiners of Professional Counselors.
The overall purpose of the Texas Administrative Code, Chapter 681 (Professional Counselors), is to implement the provisions of Texas Occupations Code, Chapter 503 (the Licensed Professional Counselor Act), concerning the licensing and regulation of professional counselors.
Texas Administrative Code - Chapter 681 (Professional Counselors)
SUBCHAPTER B (Rules of Practice)
Texas Administrative Code (TAC), Chapter 681, SUBCHAPTER B, provides the rules of practice concerning the practice of professional counseling in Texas. SUBCHAPTER B covers various topics such as setting and maintaining appropriate professional boundaries, ensuring that all actions are in the best interest of the client, maintaining confidentiality, and avoiding financial or other situations that create a conflict of interest or other professional pitfalls, to name just a few. While the rules encompass a wide variety of subjects, they share one common goal and theme: LPCs must ensure that any action they take is in the client's best interest, rather than their own.
This course focuses on most, but not all, of the sections of Chapter 681, SUBCHAPTER B, which is divided into the following sections:
RULE 681.31, Counseling Methods and Practices
The practice of professional counseling is a nuanced field that relies heavily on the use of specific methods, techniques, and modalities to effectively address the diverse needs of clients. It is imperative that these approaches are employed by professional counselors who have received appropriate training and demonstrate competency in their application. This ensures not only the ethical delivery of services but also maximizes the efficacy of the interventions used. Authorized counseling methods may include various evidence-based modalities such as cognitive-behavioral therapy (CBT), which focuses on identifying and altering negative thought patterns; person-centered therapy, which emphasizes unconditional positive regard and empathy; and solution-focused brief therapy, which targets specific goals and solutions rather than an emphasis on historical issues. Each of these methods requires a solid foundation of theoretical understanding and practical skill that can only be attained through rigorous education and supervised experience.
The dynamic nature of counseling necessitates that professionals remain aware of emerging techniques and evolving practices. This commitment to ongoing professional development ensures that counselors can offer the most current and effective therapeutic options. Adhering to ethical guidelines and professional standards is crucial; it not only protects clients but also enhances the counselor's credibility and effectiveness. Therefore, it is essential that counselors continuously engage in training and education related to their chosen modalities, as well as participate in peer supervision and consultation. Ultimately, the responsible and informed application of authorized methods fosters a therapeutic environment that promotes client growth, resilience, and well-being, reinforcing the profession's integrity and the foundational goal of facilitating meaningful change in individuals' lives.
Published in the Consolidated Rulebook, the Texas Administrative Code, section 681.31, states:
The use of specific methods, techniques, or modalities within the practice of professional counseling is limited to professional counselors appropriately trained and competent in the use of such methods, techniques, or modalities. Authorized counseling methods, techniques and modalities may include, but are not restricted to, the following…”1
Section 681.31 lists some of the authorized methods, techniques, and modalities professional counselors may use in practice. The authorized approaches mentioned in section 681.31 are not intended to be an exhaustive list. For instance, when a commenter; “requested §681.31 be amended to include EMDR as a counseling method,” the response was; “The Executive Council declines to amend §681.31 to specifically list EMDR as a counseling method. The rule is not intended to be an exhaustive list of all counseling methods, techniques, and modalities; and at this time there is not a need to add to the list of examples in this rule.”
Another point is that, just because a method or modality is listed, doesn’t mean a particular LPC has received adequate training in its use. In fact, it would be most likely impossible for a LPC to be adequately trained in the numerous counseling approaches and techniques available within all of the major theoretical categories: humanistic, cognitive, behavioral, psychoanalytic, constructionist and systemic.
Take a look at the modalities, techniques and approaches mentioned in Section 681.31. Which of these do you feel comfortable using with clients? Which ones might require additional training?
Individual counseling ● interpersonal ● cognitive ● cognitive-behavioral ● behavioral ● psychodynamic ● affective methods ● group counseling ● marriage/couples counseling ● family systems methods and strategies ● family counseling ● addictions counseling ● 12-step methods ● rehabilitation counseling ● education counseling ● career development counseling ● sexual issues counseling ● psychotherapy ● play therapy ● hypnotherapy ● music ● art ● dance movement ● techniques employing animals ● biofeedback ● formal and informal testing instruments and procedures ● consulting ● crisis counseling.
It’s important to evaluate one’s own training, experience, and competence, before using a counseling technique or approach. Practicing beyond one’s scope or without proper training is unethical. The American Counseling Association Code of Ethics provides guidance on several areas related to counseling methods and practices:
• Counselors have a responsibility to the public to engage in counseling practices that are based on rigorous research methodologies. (ACA Code of Ethics, Section C, Introduction)
• Counselors practice only within the boundaries of their competence, based on their education, training, supervised experience, state and national professional credentials, and appropriate professional experience. (ACA Code of Ethics, C.2.a.)
• Counselors practice in specialty areas new to them only after appropriate education, training, and supervised experience. While developing skills in new specialty areas, counselors take steps to ensure the competence of their work and protect others from possible harm. (ACA Code of Ethics, C.2.b.)
• Counselors accept employment only for positions for which they are qualified given their education, training, supervised experience, state and national professional credentials, and appropriate professional experience. Counselors hire for professional counseling positions only individuals who are qualified and competent for those positions. (ACA Code of Ethics, C.2.c.)
• Counselors continually monitor their effectiveness as professionals and take steps to improve when necessary. Counselors take reasonable steps to seek peer supervision to evaluate their efficacy as counselors. (ACA Code of Ethics, C.2.d.)
• Counselors take reasonable steps to consult with other counselors, the ACA Ethics and Professional Standards Department, or related professionals when they have questions regarding their ethical obligations or professional practice. (ACA Code of Ethics, C.2.e.)
• Counselors recognize the need for continuing education to acquire and maintain a reasonable level of awareness of current scientific and professional information in their fields of activity. Counselors maintain their competence in the skills they use, are open to new procedures, and remain informed regarding best practices for working with divere populations. (ACA Code of Ethics, C.2.f.)
• According to the ACA Code of Ethics; “If counselors lack the competence to be of professional assistance to clients, they avoid entering or continuing counseling relationships.” (ACA Code of Ethics, A.11.a.)
Regardless of the methods used, LPCs should be prepared to verify their training, experience, and clinical reasons for using a particular approach. In preparation to become an LPC, some counseling approaches would be adequately covered in most graduate programs, along with the required supervised work experience. Other methods might be more specialized and require additional training or certification.
The use of all modalities mentioned in 681.31 are limited to professional counselors; “appropriately trained and competent in the use of such methods, techniques, or modalities.” There are some additional requirements for a few of the techniques mentioned.
For example, according to 681.21(15), counselors using biofeedback; “must be able to prove academic preparation and supervision in the use of the equipment as part of the counselor’s academic program or the substantial equivalent provided through approved continuing education.”
LPCs who use assessment and appraisal related to testing must be in compliance with the criteria listed in Section 681.43. Consulting, according to 681.31 (17) uses; “the application of specific principles and procedures.”
Other than general terms like; “appropriately trained” and “competent,” the specifics of how a licensee would demonstrate competence for the approaches cited in Section 681.31 is not spelled out. Counselors should assume the burden of proof rests on them when demonstrating competence in a particular area.
The same type of considerations specifically mentioned for the use of biofeedback, test administration, and consulting, would be part of the many items for consideration applying to cognitive-behavioral therapy, family counseling, play therapy, or any of the many other approaches mentioned in Section 681.31.
If an LPC’s counseling methods or techniques have been questioned by a client, colleague, supervisor, or as the result of a complaint filed with the BHEC, licensees should be prepared ahead of time to provide a thorough response that includes verification of adequate training, experience, and knowledge of research, that supports the approach.
Some helpful questions to consider when determining one’s ability to treat a client, or the approach that should be used, might include the following:
• Am I practicing within the policies and procedures of the agency where I am employed?
• Can I verify that I have been trained and gained adequate experience to treat this population or diagnosis?
• Am I using methods, practices, and techniques that are up-to-date, considered best practice, and validated by research?
• If I am unsure of my competence, have I consulted with colleagues or supervisors on the matter?
• Do I have an on-going procedure in place to assess my counseling efficacy through peer supervision or consultation?
To drive home the point and importance to avoid practicing beyond one’s scope, one legal entity identified the following as two common reasons for malpractice lawsuits filed against counselors; 1) the use of techniques without proper training and; 2) failing to consult with peers or to take advice from peers.2
Not only are counselors challenged to ensure their competencies match the needs of clients at the time of admission to services, clients may present issues that emerge later on in the counseling process that may require a referral. For instance, a client may indicate a primary need for help with panic attacks and reveal several sessions later that he or she has been abusing alcohol daily.
Just as an oncologist would refer a patient with cardiac problems to a cardiologist, LPCs must continually assess the match between their own competencies and the needs of clients.
The acquisition and evaluation of up-to-date skills through additional certifications, continuing education, experience and other means, should be on-going for all counselors. A counselor’s scope of practice should always consider the client’s needs and prevent harm.
Harmful Counseling Techniques
Arguably, many counseling methods or techniques could be ineffective, ill-advised, or even dangerous, if used improperly in a given situation with a particular client. Glenys Parry, a professor and chief investigator of a government funded study in England probing the harm of some therapies, concluded that most people are helped by therapy, but added, “anything that has real effectiveness, that has transformative power to change your life, has also got the ability to make things worse if it is misapplied or it's the wrong treatment or it's not done correctly."3
Harmful counseling practices can significantly undermine the therapeutic process and negatively impact clients' mental health and well-being. One such practice is the imposition of personal beliefs and values on clients. When counselors prioritize their own perspectives over the client's lived experiences, it creates a power imbalance that can stifle open communication and discourage clients from expressing their true feelings.
Additionally, neglecting to establish a safe and supportive environment can lead to feelings of vulnerability and mistrust, further alienating individuals seeking help.
Another detrimental practice is the reliance on outdated or unverified techniques that lack empirical support. For example, implementing interventions without tailoring them to the unique context and needs of the client can obstruct progress and leave individuals feeling misunderstood or neglected.
Furthermore, a lack of cultural competence can manifest as an insensitivity to the diverse backgrounds of clients, which may alienate them and prevent beneficial engagement in the counseling process.
Finally, ignoring ethical boundaries, such as dual relationships or breaches of confidentiality, can severely damage the client-counselor relationship. Such violations erode trust and can lead to lasting harm, discouraging individuals from seeking help in the future. It is crucial for counseling professionals to remain vigilant about these harmful practices to foster a therapeutic environment that prioritizes clients' safety, respect, and empowerment.
Some occurrences of counseling malpractice illustrate the potential for severe consequences. For example, a young girl was smothered to death in a rebirthing session despite prior evidence the technique was harming the child. The unlicensed “counselor” was applying rebirthing therapy in the course of attachment therapy with aid of the girl’s mother and three assistants (Nicholson, 2001). Rebirthing has been banned in some states and opposed or not recognized as viable treatment by professional organizations in others.
The Example of Recovered Memory
The recovery of repressed memories of child abuse became popular in the early 1980’s. A wave of prosecutions and lawsuits against alleged perpetrators followed. At the same time, many children provided accounts of current or recent abuse as well.
In the 1990’s a wave of malpractice claims against counselors and organizations accused of eliciting false memories followed. The recovered memories were often elicited through manipulative interrogation techniques directed at children. The incidents were often unsupportable by evidence or even extremely improbable.
Many feel that this period constituted a modern witch-hunt. In Manhattan Beach, California, as the McMartin Preschool case was unfolding, many cars displayed bumper stickers saying, “We Believe the Children.” Smear campaigns were directed at people who questioned the recovered memory movement.
As experts came to understand the situation better, more sober discussions ensued, buoyed by research. Many recognized that it was possible to inadvertently, or purposely, manipulate children during assessments. Guidelines for interviewing children and for assessing symptoms were developed with this in mind. Much research has clarified the nature of memory, therapy, and testimony relevant to this issue.4 Successful cases against counselors using inappropriate means of producing memories of childhood abuse resulted in large penalties in the 1990s.
The wave of repressed memory and questionable abuse cases peaked in the mid 1990’s, and have diminished as a result of research and increased sophistication in the courts, social services, the public, and counseling.
Challenges of Evidence-Based Practice
The emphasis on evidence-based therapies (EBTs) in the field of counseling has increased with time. EBTs are often used to establish the evaluation of academic programs, requirements for licensure, how counselor competence is assessed, and how reimbursement policies are structured.
Researchers have pointed out the inherent limitations of randomized control trials to adequately define and measure psychological problems, the generalizability of findings, the under representation of clients with comorbid conditions, and the confounding nature and impact of psychosocial stressors on research subjects, to name a few. Nevertheless, clinicians face increasing challenges to justify their approaches in terms of evidence such as outcome studies and other research published in peer-reviewed journals5
Experts may raise concerns regarding inadequate training in evidence-based practice on the part of academic institutions. However, there are significant challenges in attempting to fulfill this aspiration.5
There can be difficulty; “converting clinical guidelines into active performance measures,” or in, “integration of findings into daily operations.”5 Research may not apply to psychotherapy in the field as well as intended. Counselors in research studies may not actually carry out therapy with as much fidelity to the prescribed method as is believed, because they may put clients’ needs ahead of the research objectives, or because the client cohort is not as homogenous as they appeared to be during enlistment of subjects.
Often, there is not enough consistent data available to form a secure evidence-based opinion, despite the existence of practice guidelines and texts that synthesize what information is available. Research can’t always keep up with clinical innovation and the diversity of clients.
Staying up-to-date is the first priority in evidence-based practice. However, it is important to remember that the integrity of research is often limited by problems such as bias and weak methods. Statistically weak results may be presented as though they are newsworthy.
As a result, many methods must gain credibility through clinical experience. However, licensees can avoid acting on blind faith by staying outcome-focused. We must carefully assess risks and our own scope of practice and competence.
RULE 681.35
Informed Consent
Informed consent is a foundational aspect of ethical counseling, ensuring that clients are fully aware of the services they will receive, the risks involved, and their rights in the therapeutic relationship. However, there are instances where counselors have failed to uphold the standards set forth in regulations in Texas Administrative Code (TAC) 681.41. For example, a counselor working in a school setting failed to inform a student and their parents about the nature of the counseling services, including the limitations of confidentiality and the potential for information sharing. This oversight led to a breach of trust when sensitive information was later disclosed without parental consent.
Another example involves a private practice counselor who did not provide clients with clear information about therapy fees, session duration, and the overall treatment process. This lack of transparency left clients feeling misled and uncertain about their financial commitment and expectations for treatment, ultimately jeopardizing the therapeutic alliance. Additionally, a marriage and family therapist neglected to explain the implications and risks associated with couple’s therapy, particularly regarding how individual sessions might affect the dynamics of the relationship. This failure to provide adequate informed consent led to conflict and dissatisfaction among the couple as they struggled with unresolved issues that were not addressed in therapy.
Lastly, a counselor specializing in substance abuse recovery failed to adequately inform clients about the potential consequences of disclosing personal information during group therapy sessions. The counselor did not emphasize that confidentiality could not be guaranteed in such a setting, which resulted in several participants feeling exposed and vulnerable after their experiences were shared outside the group by other members. These examples underscore the critical importance of thorough and clear informed consent practices in counseling, as failure to comply can lead to significant consequences for both clients and practitioners.
In Texas, there are certain requirements that must be met by licensees before a professional relationship is established and counseling services can begin. According to TAC 681.41, regardless of the setting, licensees must provide counseling only in the context of a professional relationship. This includes having clients complete an informed consent, signed written receipt of information, or in the case of involuntary treatment a copy of the appropriate court order.
Other requirements of informed consent include the following:
(1) fees and arrangements for payment;
(2) counseling purposes, goals, and techniques;
(3) any restrictions placed on the license by the Council;
(4) the limits on confidentiality;
(5) any intent of the licensee to use another individual to provide counseling treatment intervention to the client;
(6) supervision of the licensee by another licensed health care professional including the name, address, contact information and qualifications of the supervisor;
(7) the name, address and telephone number of the Council for the purpose of reporting violations of the Act or this chapter; and
(8) the established plan for the custody and control of the client's mental health records in the event of the licensee's death or incapacity, or the termination of the licensee's counseling practice.
Rule 681.35 also states:
(b) A licensee must inform the client in writing of any changes to the items in subsection of this section, prior to initiating the change.
(c) Prior to the commencement of counseling services to a minor client who is named in a custody agreement or court order, a licensee must obtain and review a current copy of the custody agreement or court order, as well as any applicable part of the divorce decree. A licensee must maintain these documents in the client's record and abide by the documents at all times. When federal or state statutes provide an exemption to secure consent of a parent or guardian prior to providing services to a minor, a licensee must follow the protocol set forth in such federal or state statutes.
(d) A licensee acting within the scope of employment with an agency or institution is not required to obtain a signed informed consent, but must document, in writing, that the licensee informed the client of the information required by subsection (a) of this section and that the client consented.
These requirements are some of many that help inform clients about the nature of the relationship and the obligations of the counselor. Some of the items may take a few minutes to explain. Others, for instance; “counseling purposes, goals, and techniques,” may require on-going explanation and re-evaluation throughout the counseling process. These are just some of the many aspects that help to create and maintain a professional relationship with clients.
Informed consent involves the clear and thorough explanation of all services provided. It is an on-going process. In addition to the areas mentioned above, other areas to consider for the informed consent process include the following:
• Qualifications of Counselor(s)
• Eligibility of client for services
• Counseling Sessions/Missed or Late Cancelation Appointments
• Risks of Counseling
• The Boundaries of a Therapeutic Relationship
• Electronic Communication
• Your Rights as a Client
• Cooperation of Client
• Rates
• Insurance
• Miscellaneous Fees
• Referrals
• Records
• After-Hours Emergencies
• Therapist’s Incapacity or Death
• Acknowledgment and Statement of Understanding
• Client Satisfaction Surveys
• The nature and purpose of treatment
• Potential benefits of treatment
• Limits to treatment
• Treatment alternatives
• Risks associated with not receiving treatment
• The clients’ right to refuse to consent or to revoke their consent at any time
ADDITIONAL ASPECTS OF A PROFESSIONAL RELATIONSHIP
One of the main purposes of Chapter 681 is to help licensees adopt practices that maintain a professional relationship with clients. Anytime a counselor decides to make the relationship something other than a professional one, there is greater potential for harm to the client.
It could be argued that almost every topic or situation codified in Chapter 681 is intended to safeguard the professional relationship from becoming something other than therapeutic for the client.
PROFESSIONAL VALUES
A professional relationship requires professional values to be upheld by the licensee. In order for something to have value, it has to be important and something to which we are committed. Ethical decisions are much more likely to be one’s approach if there is a commitment to live out our commitment to work in the client’s best interest.
The ACA Code of Ethics Preamble identifies the following as core professional values:
enhancing human development throughout the life span; honoring diversity and embracing a multicultural approach in support of the worth, dignity, potential, and uniqueness of people within their social and cultural contexts; promoting social justice; safeguarding the integrity of the counselor–client relationship; and practicing in a competent and ethical manner.
While professional values are internal, they are the root and motivation of principles we demonstrate externally through our actions. According to ACA, the fundamental principles of professional ethical behavior are:
The ACA’s fundamental principles include:
-Autonomy, or fostering the right of the client to control the direction of one’s life;
-Nonmaleficence, or avoiding actions that cause harm to the client;
-Beneficence, or working for the good of the individual and society by promoting mental
health and well-being;
-Justice, or treating individuals equitably and fostering fairness and equality;
-Fidelity, or honoring commitments and keeping promises, including fulfilling one’s responsibilities of trust in professional relationships; and
-Veracity, or dealing truthfully with individuals with whom counselors come into professional contact.
FIDUCIARY RESPONSIBILITY
Many different kinds of relationships, particularly professional relationships, involve a fiduciary duty. A fiduciary duty is a duty imposed, generally, on the more powerful party to act in the best interest of the less powerful party. A lawyer, for example, has a fiduciary duty to her clients, who place their trust and confidence in her hands; she has special expertise they do not, and they retain her and pay her fees with the understanding that she will use that expertise to represent their interests.
Similarly, a physician has a fiduciary duty to his patients: They seek her medical advice because she has the specialized knowledge and skill necessary to deal with their health problems in ways that they cannot – and, again, they pay her fees in the expectation that she will use that knowledge and skill to make them well.
Fiduciary responsibility comes in many forms. Fiduciaries include physicians, attorneys, teachers, financial advisors, parents, real estate agents, and just about anyone who owes a duty of care, loyalty, good faith, confidentiality, prudence, and disclosure to someone.
As mentioned throughout this course, the primary objective of counselor ethics is to protect clients and work in their best interests to assist them in meeting their counseling goals. The ACA identifies one of the purposes of its Code of Ethics to be the following: “The Code serves as an ethical guide designed to assist members in constructing a course of action that best serves those utilizing counseling services and establishes expectations of conduct with a primary emphasis on the role of the professional counselor.”
Fiduciary responsibility may include the following:
Duty of Care: This pertains to being competent to provide the help clients need. It involves sound judgment in making decisions to assist the client. It offers options that reflect sensible decision-making. This means that LPCs must engage in continuous education and training to enhance their skills, enabling them to apply sound judgment in assessing clients' needs. By offering well-considered options that reflect prudent decision-making, counselors help clients navigate their challenges with informed guidance.
Duty of Loyalty: This pertains to acting in the best interest of the beneficiary at all times and correcting any possible conflicts of interests. Duty of Loyalty mandates that LPCs prioritize their clients' interests above all else. This involves actively identifying and correcting any potential conflicts of interest that may arise during the therapeutic relationship. By maintaining unwavering loyalty, counselors foster an environment built on trust, assuring clients that their welfare is paramount.
Duty of Good Faith: Licensees always act to the benefit of the client and within the confines of the law. Duty of Good Faith requires counselors to act honestly and ethically, consistently pursuing actions that benefit clients while adhering to legal stipulations. This duty reinforces the integrity of the counseling profession, creating a framework within which clients can confidently explore their thoughts and emotions.
Duty of Confidentiality: Confidentiality is the cornerstone of the counseling relationship. It is never violated except when it is required by law in specific situations. LPCs must rigorously protect the privacy of their clients, disclosing information only when legally mandated or ethically justified. By safeguarding this sensitive information, counselors build a strong rapport with clients, encouraging openness and vulnerability.
Duty of Prudence: Fiduciaries use good judgment and carefully weigh the risks of any decisions impacting the client. The Duty of Prudence compels LPCs to exercise careful judgment when making decisions that affect their clients. This involves weighing potential risks and benefits to ensure that the client's best interests are always front and center.
Duty to Disclose: Fiduciaries are transparent with clients in disclosing information that can impact clients and their ability to carry out their duties. The Duty to Disclose mandates transparency between counselors and clients. LPCs must communicate relevant information that could impact clients' understanding of their treatment and the counselor's professional obligations. By ensuring that clients are well-informed, counselors empower them to make educated choices about their therapeutic journey.
Collectively, these fiduciary responsibilities ensure that Texas LPCs provide ethical, effective, and client-centered care, fostering a therapeutic alliance that is both supportive and constructive.
RULE 681.36
Client Records
In the practice of licensed counseling and therapy, meticulous record-keeping is essential to ensure that each client receives appropriate care and that the therapist complies with legal and ethical guidelines. For each client, a licensee must maintain accurate records that include various critical documents. For instance, the signed informed consent is fundamental, reflecting the client's understanding and agreement to the treatment process. In cases of involuntary treatment, a copy of the court order is necessary to validate the intervention. Additionally, the intake assessment provides a comprehensive overview of the client's psychological and emotional state upon entry into the program.
Furthermore, documenting the dates of counseling treatment interventions is crucial for both tracking progress and scheduling future appointments. Effective treatment often relies on specific methodologies; therefore, licensees need to record principal treatment methods employed during sessions, such as cognitive-behavioral therapy or motivational interviewing. Progress notes are also integral to monitoring the client’s development and adapting the treatment plan as necessary. Each client record must include a detailed treatment plan that outlines the therapeutic goals and strategies tailored to the individual's needs. Lastly, accurate billing information is vital for ensuring that the practice complies with financial regulations and for clear communication with clients regarding the cost of services.
In terms of record retention, it is important to note that, in the absence of specific state or federal laws, records must be maintained for a minimum of seven years following the termination of services. Alternatively, if a client reaches the age of majority, records should be kept for five years after that date, whichever period is longer. This guideline is designed to safeguard client information and ensures that relevant data remains available for any future consultations or legal matters.
Additionally, records generated by a licensee during their employment with an agency or institution are typically maintained by the respective employer. However, if the employer does not retain these records, it becomes the responsibility of the licensee to ensure they are preserved and managed appropriately. This stipulation emphasizes the importance of organizational protocols in handling sensitive client information while placing responsibility on individual licensees to uphold ethical and professional standards in their practice.
RULE 681.37
Billing and Financial Arrangements
Billing requirements play a crucial role in ensuring transparency and integrity within therapeutic and counseling practices. For instance, a licensee must charge clients solely for services that have been rendered or for services that both the client and the licensee explicitly agreed upon at the onset or through mutual written modifications. An example of proper billing would be a therapist who provides weekly sessions and closely documents the enhancements to the treatment plan that may necessitate additional sessions, thus adequately reflecting all charges on the billing statement.
Additionally, clients and their guardians have the right to request a plain-language explanation of previous charges made for counseling services. For example, if a parent requests this information for their minor child, the licensee must provide a clear breakdown of each treatment charge, avoiding any jargon or technical terms that might confuse the client or guardian. This practice supports informed consent and empowers the client or guardian to understand the financial implications of the treatment received. It should also be noted that overcharging clients is strictly prohibited; hence, a licensee who charges higher than the agreed fee for a session or service could face ethical and legal repercussions. Furthermore, licensees are not allowed to submit bills for treatments that they know or should know are unwarranted. This might include billing for a service that, upon reflection, does not align with the client's treatment goals or was never actually administered, although cancellations may be billed accordingly.
In addition to billing integrity, the ethical considerations extend into relationships with potential referral sources. Under Texas law, a licensee is prohibited from offering or accepting any form of remuneration for securing or soliciting clients. This regulation ensures that the focus remains on providing the best care to clients without the interference of financial incentives that could lead to conflicts of interest.
Licensees working under contracts with chemical dependency or mental health facilities must also comply with specific stipulations outlined in the Texas Health and Safety Code regarding solicitation and contracting practices. By following such stringent guidelines, licensees ensure their practices adhere to state laws regarding marketing and remuneration, fostering a safe and ethical environment for client care.
NOTE: In the Rulebook dated March 24,2025, the following has been deleted from Rule 681.37 regarding Billing and Financial Arrangements at the end of paragraph (c) in green highlight:
(c) A licensee employed or under contract with a chemical dependency facility or a mental health facility must comply with the requirements in the Texas Health and Safety Code, §164.006, relating to soliciting and contracting with certain referral sources. [Compliance with the Treatment Facilities Marketing Practices Act, Texas Health and Safety Code Chapter 164, will not be considered as a violation of state law relating to illegal remuneration.]
Reasoned Justification.
The adopted amendments remove language identified during the quadrennial rule review to better align with the agency's statute.
RULE 681.38
Conflicts, Boundaries, Dual Relationships and Termination of Relationships
"A licensee must not engage in activities for the licensee's personal gain at the expense of a client."
Texas Administrative Code 681.38(a) establishes a crucial ethical standard for licensed professionals, emphasizing the importance of prioritizing client welfare above personal interests. This regulation mandates that licensees must refrain from engaging in any activities that could benefit themselves financially or otherwise at the expense of their clients. For instance, a therapist must avoid the temptation to recommend unnecessary treatments or sessions solely to increase their income, instead focusing on the client's best therapeutic interests.
681.38(a) acts as a fundamental guideline that reinforces the ethical responsibilities of licensees, fostering a professional environment where clients’ welfare is the top priority.
According to paragraph (b), a licensee is permitted to promote their personal or business activities to clients if these offerings are designed to enhance the counseling process or assist clients in reaching their counseling objectives. However, before initiating any engagement related to these activities, the licensee is required to disclose their personal or business interests to the client transparently. This disclosure is crucial to maintain ethical standards and ensure that clients are fully informed about any potential conflicts of interest. Moreover, the licensee must avoid exerting undue influence when encouraging clients to consider these activities, services, or products, thereby safeguarding the clients' autonomy and decision-making in the counseling relationship.
(c) A licensee must set and maintain professional boundaries.
Professional boundaries encompasses many aspects of behavior for Texas licensed professional counselors. Professional boundaries include essential components that ensure the integrity of the therapeutic relationship and the well-being of clients. These boundaries delineate the space between the counselor's professional responsibilities and personal inclinations, safeguarding the client from potential harm and exploitation.
Counselors must maintain a clear distinction between their professional roles and personal relationships, avoiding dual relationships that could impair their objectivity or create conflicts of interest. For instance, engaging in social interactions with clients outside the therapeutic setting or providing services to friends or family can jeopardize the therapeutic alliance and undermine the counselor's effectiveness.
In Texas, licensed professional counselors are also mandated to adhere to professional boundaries that emphasize respect for clients’ autonomy and confidentiality. This includes obtaining informed consent before sharing any information about the client with third parties. Counselors must also be attentive to their own vulnerabilities and biases, as these elements can inadvertently skew the counseling process. Establishing professional boundaries helps create a safe and supportive environment for clients to explore their thoughts and feelings, fostering trust and promoting therapeutic progress.
Furthermore, Texas licensed professional counselors are expected to maintain appropriate limits in their interactions with clients, particularly concerning physical touch, personal disclosures, and emotional support. These boundaries not only protect clients but also help counselors manage their own emotional states and prevent burnout. Counselors should engage in regular supervision and reflection to assess how they are managing these boundaries, ensuring that they remain attuned to the needs of their clients while safeguarding their own well-being and professional integrity. Upholding these professional boundaries is crucial in fostering a therapeutic environment that promotes healing, growth, and positive change.
Included in professional boundaries is the prohibition against non-therapeutic relationships with clients. The distinction between therapeutic and non-therapeutic relationships is crucial. A non-therapeutic relationship refers to any interaction that occurs outside the scope of counseling, whether initiated by the client or the licensee.
Such relationships can blur the lines between professional and personal boundaries, potentially complicating the therapeutic process. Because of the inherent power dynamics and potential for exploitation in a client-licensee relationship, ethical guidelines stipulate that a counselor may not engage in a non-therapeutic relationship with a client for a minimum of two years after the formal counseling relationship has concluded. This waiting period is designed to protect the integrity of the counseling framework and ensure that the client is not vulnerable during a critical transitional phase.
Moreover, specific prohibitions apply to romantic or sexual relationships with clients, which must remain off-limits for five years after the conclusion of the counseling relationship. Recognizing the emotional intensity and potential dependency that can arise during therapy, this extended period aims to safeguard the client's well-being and mitigate any risk of exploitation or coercion. If a licensee wishes to engage in a non-therapeutic relationship after this period, they carry the burden of proof to demonstrate that the relationship was consensual and not manipulative. Additionally, they must show that the relationship is not detrimental to the client, taking into consideration various factors outlined in regulatory guidelines.
Finally, ethical standards dictate that a licensee must refrain from providing counseling services to family members, personal friends, educational associates, or business associates. This policy prevents conflicts of interest and ensures that professional boundaries remain intact. By maintaining these boundaries, counselors can uphold the trust and safety necessary for effective therapeutic interventions, ultimately prioritizing the client's mental health and welfare over personal or familial connections.
Additional professional boundaries included in Rule 681.37 states that Texas LPCs are prohibited from giving or receiving gifts valued at more than $50. Additionally, licensees must refrain from borrowing or lending money or items of value to clients or their relatives. Furthermore, the acceptance of payment in the form of goods or services instead of monetary compensation is also forbidden. These regulations are designed to foster trust and transparency in client interactions, ultimately protecting both the client and the professional's integrity.
Licensees are prohibited from engaging in non-professional relationships with a client's family members or individuals connected to the client if such relationships could harm the client. This guideline underscores the importance of safeguarding the client's well-being by preventing conflicts of interest and emotional complications.
Seeing More Than One Therapist
Licensees must refrain from providing counseling to individuals who are already receiving therapy from another mental health provider unless they have the knowledge and consent of that provider. This requirement emphasizes the need for collaboration among professionals to ensure that the client receives comprehensive care without conflicting interventions. If the licensee discovers that a client is undergoing concurrent therapy, they must seek the client's permission to communicate with the other professional, aiming to foster positive and cooperative relationships.
A licensee who is willing to treat a client concurrently with another counselor must first obtain permission from the other clinician. Clients should not receive concurrent counseling without both therapists’ approval.
There could be situations when a client fails to tell one or both therapists of the concurrent treatment, but if it is discovered, the licensees must seek release from the client to work collaboratively.
The licensee must not knowingly offer or provide counseling to an individual concurrently receiving counseling treatment intervention from another mental health services provider except with that provider's knowledge. If a licensee learns of such concurrent therapy, the licensee must request release from the client to inform the other professional and strive to establish positive and collaborative professional relationships.
The American Counseling Association’s Code of Ethics is similar:
When counselors learn that their clients are in a professional relationship with other mental health professionals, they request release from clients to inform the other professionals and strive to establish positive and collaborative professional relationships. (A.3.)
There are no laws or regulations that strictly prohibit a client from seeing one or more therapists at the same time. Some clients believe they benefit from the arrangement, but the monetary cost alone would prevent many from doing so.
The practice of using multiple therapists can be a part of strategic counseling services. The licensee may believe the client would benefit from a specialized approach used by another counselor to address certain issues, but would like to continue treatment with the client to address other issues. Clients with dual diagnoses might especially present these kinds of treatment scenarios.
Some therapists are opposed to concurrent therapy. The potential for incongruent objectives, splitting by the client, extra time required for collaboration with another counselor, or problems working through transference with the client, might be a few reasons for opposing it. Although not entirely analogous, they may see it as similar to a client seeing multiple prescribers of medication for the same condition.
In summary, concurrent therapy may be beneficial for some clients as long as the two professionals agreed to it, respect professional boundaries, and work collaboratively so the client does not receive conflicting or confusing advice.
Furthermore, a licensee is obligated to terminate a professional counseling relationship if it appears that the client is not benefiting from the sessions. This commitment to client welfare requires the counselor to be vigilant about the effectiveness of their methods and to prioritize the client’s best interests.
When termination of the relationship becomes necessary, the licensee must take proactive steps to facilitate the client's transfer to appropriate care, ensuring continuity and support in the pursuit of mental health. These guidelines collectively highlight the ethical responsibility of counselors to maintain professional integrity and prioritize the well-being of their clients throughout the therapeutic process.
More on Professional Relationships
In general, a professional relationship is one in which the parameters and goals of the relationship are clearly defined, understood, and agreed upon by the licensee and client. A professional relationship is one in which the licensee always works for the best interests of the client.
According to the Texas Administrative Code, Licensed Professional Counselors (LPCs) are required to provide counseling exclusively within the framework of a professional relationship. This regulation emphasizes the importance of establishing a structured and ethical connection between the counselor and the client, which is essential for effective therapeutic work. A professional relationship is characterized by clear boundaries, mutual respect, and trust, creating a safe environment where clients can explore their thoughts, feelings, and behaviors. Such a setting not only facilitates the therapeutic process but also safeguards both the counselor and the client from potential conflicts of interest and ethical dilemmas.
The American Counseling Association (ACA) further elaborates on the essence of counseling by defining it as a professional relationship designed to empower diverse individuals, families, and groups. This definition highlights the multifaceted nature of counseling, which encompasses not only mental health support but also guidance in wellness, education, and career aspirations. This empowerment is particularly crucial in a diverse society where individuals face varying challenges and barriers. The professional relationship fosters an atmosphere of collaboration, enabling clients to set and achieve personal goals while receiving tailored support that respects their unique backgrounds and experiences. By adhering to these principles, LPCs uphold the integrity of the counseling profession and contribute to the overall well-being of their clients.
Moreover, the stipulation that counseling activities must occur within a professional context serves to reinforce the ethical standards upheld by the counseling profession. It acts as a safeguard against the potential for dual relationships that could complicate the therapeutic process and undermine the trust essential for effective counseling. For example, engaging in social or personal relationships with clients outside the counseling sessions could lead to biases, exploitation, or breaches of confidentiality. Therefore,
Texas LPCs must navigate carefully the boundaries of professional relationships, ensuring that their practice not only adheres to legal regulations but also aligns with the core values of respect, integrity, and professionalism as outlined by organizations like the ACA. In doing so, they enhance the effectiveness of their interventions and the overall quality of care provided to their clients.
Non-Therapeutic Relationships
The TAC defines a non-therapeutic relationship as: any non-counseling activity initiated by either the licensee or client that results in a relationship unrelated to therapy.
It does not take a great deal of discernment to understand the predicament in which licensees could find themselves by choosing to engage in a non-therapeutic relationship with a current or former client, or engaging in sexual exploitation or sexual contact with a client, former client, LPC Associate, or student.
As already mentioned, the TAC defines ‘non-therapeutic’ as any non-counseling activity initiated by either the licensee or client that results in a relationship unrelated to therapy. The line between ‘therapeutic’ or ‘non-therapeutic’, as well as ‘related to counseling’ or ‘not related counseling’, might be straight forward in most cases, but not all.
For instance, some licensees would consider visiting a client in the hospital, or attending a client’s wedding or graduation, to be therapeutic and related to therapy. Other licensees might feel uncomfortable doing so in almost all cases. Much would depend on the context and the relevant factors already cited. The ACA Code of Ethics mentions all of these examples (weddings, graduations, funerals) as potentially permissible within the therapeutic relationship, as long as certain precautions are taken.
Set standards for acceptable behavior within the professional relationship include within them an allowance for certain situations that may fall outside a typical professional relationship. However, these situations, if ventured into, may be permissible, but potentially require considerable justification by the licensee.
When boundaries are extended for certain events as weddings or funerals, the ACA Code of Ethics advises counselors to “take appropriate professional precautions such as informed consent, consultation, supervision, and documentation to ensure that judgment is not impaired and no harm occurs.”
In addition, the ACA Code advises that, when counselors extend boundaries, they must officially document, prior to the interaction (when feasible), the rationale for such an interaction, the potential benefit, and anticipated consequences for the client or former client and other individuals significantly involved with the client or former client.
The burden of proof rests on the licensee to justify any relationship outside normal counseling parameters cited in TAC and all other applicable laws.
POTENTIAL HARM OF DUAL RELATIONSHIPS
The primary concern about dual roles played by a therapist is the potential (or actual) damage that is done to the client as a result of crossing or violating boundaries (both sexual and non-sexual). Wheeler and Bertram describe five categories where this damage may be seen6:
• Loss of objectivity or clarity. Dual relationships can add a layer of distraction to a professional relationship that is inherently already filled with challenges to objectivity and clarity. Most mental health professionals recognize that counseling and psychotherapy are subjective endeavors. Objectivity is not really possible: Perception is influenced by a host of conscious and unconscious, social, cultural, political, and life experiences variables. During graduate training, post-degree supervision, and ongoing colleague consultation, counselors are constantly striving to maintain as much clarity as possible in interacting with clients. The loss of objectivity/clarity may be consciously recognized by the counselor, or it can occur below the counselor’s awareness. In any event, the loss of objectivity and clarity represents a dynamic in the counseling office that prevents the counselor from being fully present for the client and challenges the ethically mandated primary responsibility of the counselor to respect the dignity and promote the welfare of clients. Dual relationships represent another layer of distraction that a counselor must sort through in order to maintain an acceptable level of objectivity and clarity.
• Potential for misunderstanding. Misunderstanding between human beings is natural and inevitable. Under normal circumstances, misunderstandings that occur within a counseling relationship can be worked through and often can become important diagnostic and therapeutic opportunities. When a counseling relationship is intertwined within a dual relationship there is increased opportunity for misunderstanding. Interactions that occur in the nonclinical relationships can create misunderstanding within the counseling relationship and vice versa. In human interactions, misunderstandings can quickly multiply, with one misunderstanding feeding on another until there is a breakdown of the counseling relationship. We are ethically charged to do no harm and whenever possible to minimize or to remedy unavoidable or unanticipated harm; misunderstanding fueled by a dual relationship frequently can be a conduit to client harm.
• Conflict of Interest. Co-occurring or sequential dual roles can create a conflict of interest, a situation in which a counselor (or someone or something important to the counselor) can be affected by decisions or behaviors in the client is contemplating. A conflict of interest can tempt a counselor to use the power of the counseling relationship to sway the client in a direction preferred by the counselor. Such inappropriate influence can easily result in harm to the client. Even if the counselor resists the temptation to inappropriately influence the client, the treatment relationship can still be affected. The client may wonder about the counselor’s motives, and the counselor might have some conflicted feelings for having to defer his or her own best interest in favor of the client’s.
• Breach of confidentiality and privacy. When clinical and nonclinical roles become intertwined, it becomes difficult for counselors to remember what information may be discussed. When non-counseling roles are informal or intense (friendships, social groups, business or work relationships, etc.), the likelihood of a breach of confidentiality and a violation of the client’s right of privacy dramatically increases.
• Exploitation. Mental health professionals who intentionally misuse the power differential inherent within the counseling relationship to take advantage of a client or former client are behaving in an abusive and exploitive manner. These situations tend to be the most ethically and legally egregious and often involve sexual or financial exploitation. These dual relationships are not innocent; they are not just a momentary lapse in judgment. They are the basis for real harm to the client as well as ethical and legal consequences to the counselor, including ethics complaints, licensing board disciplines, malpractice lawsuits, and possibly felony imprisonment.”
Dual relationships can include sharing meals with a client; visiting a client's home; inviting the client to visit one's own home; socializing at a party, sporting event, or other activity; or other professional or employment-related affiliations.
Experts counsel LPCs not to see clients outside of the consulting context and to avoid development of social relationships that can adversely affect the therapeutic process. Likewise, LPCs should not accept as a client any individual with whom the LPC has previously interacted in a social context.
RULE 681.41
General Ethical Requirements
Honest and accurate representation of one’s credentials, abilities, and possible outcomes with clients is essential for licensees. There are varying degrees of claims that can mislead or injure clients. “Stretching the truth” is not a minor issue. Think how even a misleading statement in a casual conversation with a colleague or friend can injure the trust we have in them and their abilities.
Clients served by counselors are often in a heightened position of vulnerability and need protection from deceptive statements about how they will respond to treatment. A depressed client who has been misled into believing a particular approach is certain to work may assume it is their fault that they have not responded as promised, or may lose hope that another approach might help.
Rule 681.41 prohibits licensees from exaggerating their credentials or expressing certitude that they can help a client. Licensees must present themselves and their services with much discretion.
According to 681.41 (a), A licensee must not make any false, misleading, deceptive, fraudulent or exaggerated claim or statement about the licensee’s services, including, but not limited to:
1) the effectiveness of services;
2) the licensee’s qualifications, capabilities, background, training, experience, education, professional affiliations, fees, products, or publications; or
(3) the practice or field of counseling.
In the context of Texas Licensed Professional Counselor (LPC) claims, exaggerated assertions can significantly undermine the integrity of the profession and violate the Texas Administrative Code, which mandates that LPCs must not misrepresent their qualifications or the effectiveness of their services. Exaggerated claims can manifest in various forms, such as overstating the efficacy of therapeutic interventions, misrepresenting credentials, or making unfounded assertions about treatment outcomes.
One pertinent example involves LPCs who may claim that their therapeutic methods guarantee specific outcomes, such as complete resolution of mental health issues within a predetermined timeframe. This type of claim is misleading and unsupported by empirical evidence, as therapeutic outcomes can vary widely among individuals.
Research indicates that exaggerated claims in health-related contexts can misinform the public and lead to unrealistic expectations regarding treatment efficacy (Bratton et al., 2019; Sumner et al., 2016). Such practices can erode trust in the counseling profession and violate ethical standards set forth in the TAC.
Another example of exaggerated claims can be found in LPCs who assert that their qualifications or experiences are superior to those of their peers without substantiating such claims. This is particularly concerning in a field where the perception of competence can significantly influence client choices. Studies have shown that exaggeration in professional credentials can lead to a loss of public trust, as it creates a false narrative about the provider's capabilities (Shyagali et al., 2022).
The TAC explicitly prohibits LPCs from making misleading statements about their qualifications, emphasizing the importance of honesty in professional representation. Moreover, LPCs may sometimes engage in "spin" by presenting their services in a manner that suggests they are more effective than they are in reality. For instance, a counselor might highlight only positive client testimonials while neglecting to mention cases where clients did not achieve desired outcomes. This selective reporting can create a skewed perception of the counselor's effectiveness, which is a violation of the ethical guidelines outlined in the TAC (Shyagali et al., 2022).
The implications of such exaggerations are profound, as they can lead clients to make ill-informed decisions regarding their mental health care.
Rule 681.41(b) states that these same requirements apply to statements the licensee makes about services provided by any mental health organization, agency, including, but not limited to, the effectiveness of services, qualifications, or products. For instance, a counselor may take pride in working for an employer that endorses CBT as their primary counseling modality. The counselor may have personally benefitted greatly from CBT and believe firmly in its use.
Despite the success of CBT and the research to validate its efficacy, it is still dependent on factors that frequently change; the motivation level of the client, or the ever-changing expertise of counselors, for example. To characterize an entire organization as effective or successful would be a highly difficult assertion to prove given all of the variables impacting such a claim.
Rulue 681.41 (c) and (d)
NOTE: Rules 681.41 (c) and (d) have been deleted in the BHEC/LPC Rulebook, March 24, 2025 edition with paragrapch (e) on Technology now moving up to paragraph (c).
The deleted paragraphs are worth noting:
[(c) A licensee must discourage a client from holding exaggerated or false ideas about the licensee's professional services, including, but not limited to, the effectiveness of the services, practice, qualifications, associations, or activities. If a licensee learns of exaggerated or false ideas held by a client or other person, the licensee must take immediate and reasonable action to correct the ideas held.]
[(d) A licensee must make reasonable efforts to discourage others whom the licensee does not control from making misrepresentations; exaggerated or false claims; or false, deceptive, or fraudulent statements about the licensee's practice, services, qualifications, associations, or activities. If a licensee learns of a misrepresentation; exaggerated or false claim; or false, deceptive, or fraudulent statement made by another, the licensee must take reasonable action to correct the statement.]
The reason given for the change is stated in the Preamble of the Texas Administrative Code:
Reasoned Justification.
The adopted amendments remove language identified during the quadrennial rule review as potentially unenforceable, while not changing the substantive requirement that a licensee not make or benefit from false, misleading, deceptive, fraudulent, or exaggerated claims.
List of interested groups or associations against the rule.
None.
Summary of comments against the rule.
Four individuals commented against the proposed rule, suggesting that it is important for license holders to correct misinformation when they learn of it. Several commenters mentioned the danger of false information appearing online, including fake online reviews.
List of interested groups or associations for the rule.
None.
Summary of comments for the rule.
One commenter supported the proposed amendment without comment.
Agency Response.
The agency appreciates the public comment. The proposed amendment will eliminate blanket language requiring a licensee to correct misrepresentations made by another person without any evidence of impact to the licensee or a client. However, Council rules will continue to prohibit a licensee from benefiting from any false, deceptive, or fraudulent statements, which would include having someone post false advertisements online. (From the Texas Register, Preamble, regarding Rule 681.41)
The Rule did not clearly distinguish between “other person” mentioned in the paragraph (c) and “others whom the licensee does not control” in paragraph (d), but it might be assumed that “other person” refered to those with whom the counselor had some control and influence, while “others whom the licensee does not control” would pertain to any other third party. Regardless, these two paragraphs have been deleted due to their difficulty to enforce.
Promoting Hope Without Misleading Statements
It is necessary to instill hope in clients. Although promoting hope is an integral part of a licensee’s role, it is important not to violate ethical standards through statements that assert outcomes for a specific client. Such statements are, in essence, unvalidated predictions of how the client will respond to treatment.
Avoiding statements that reach too far in promoting or claiming the benefit of counseling or a particular technique can be a challenge for even well-intentioned therapists who may be enthusiastic to help, have seen many individuals under their care respond favorably to counseling, who feel confident in their abilities, and want to convey hope that the client’s situation can improve with counseling.
Regardless of a counselor’s success with previous clients, there are many variables that make future results unpredictable. The benefits of counseling can be dependent on factors such as the skill of the counselor, the client’s investment in homework assignments, the client’s compatibility with, and confidence in the counselor, the client’s family support, other emerging or changing stressors faced by the client, among others.
These factors are unique for each client and invalidate absolute claims or predictions regarding a specific individual’s future success resulting from counseling interventions.
Statements like; “CBT has been effective in treating depression for many people” is an accurate claim, but; “I know you will get better with CBT,” is an unethical claim.
When clients question or report that a particular technique, or that counseling in general, is not working for them, counselors may be tempted to defend an approach with general evidence that may mislead the client to believe the approach is a guarantee of success for them personally.
In such situations, counselors can make statements like; “It has been my experience, and research demonstrates, that this approach has helped some people, but it doesn’t mean it will help you. We can wait to see if practicing some of the coping skills outside of our sessions will help, or we can try a different approach if you would like.” Or, depending on the situation, it might be time to suggest a referral to another counselor if the client suggests it or is not benefitting from treatment.
Rule 681.41 (c)
Technology
Rule 681.41 (c) states: “Technological means of communication may be used to facilitate the therapeutic counseling process.” This rule recognizes the evolving landscape of communication technology and its integral role in facilitating the therapeutic counseling process. This provision allows licensed counselors to embrace various technological means, such as video conferencing, online messaging, and telephonic consultations, to enhance the accessibility and efficiency of mental health services. By incorporating these tools, counselors can reach a broader audience, including individuals in remote areas or those with mobility challenges, thus breaking down barriers to access.
The use of technology in counseling not only expands service delivery options but also supports the therapeutic relationship between counselors and clients. When utilized effectively, these technological means can foster engagement and provide a comfortable environment for clients, especially those who may be apprehensive about traditional face-to-face interactions. However, the code emphasizes the importance of maintaining professional standards, ensuring confidentiality, and adhering to ethical guidelines. Counselors must be trained in the appropriate use of these technologies, ensuring that they safeguard client information and provide a secure platform for communication.
Moreover, this provision highlights the necessity of being adaptable in the face of ongoing societal changes, such as the increased demand for remote mental health services exacerbated by public health crises. By sanctioning the use of technological means, Texas Administrative Code 681.41(e) effectively encourages counselors to innovate and integrate modern practices into their work, ultimately enhancing the overall effectiveness of therapeutic interventions and promoting better mental health outcomes for clients across the state.
Rule 681.41 (d)
Reporting Imminent Danger
Texas licensed professional counselors are generally required to keep their clients' communications and records confidential. However, they may disclose this information if they believe the client is a danger to themselves or others. Chapter 681.41, paragraph (d) states:
A licensee may take reasonable action to inform medical or law enforcement personnel if the licensee determines there is a probability of imminent physical injury by the client to the client or others, or there is a probability of immediate mental or emotional injury to the client.
The text addressing this is Chapter 611, Section 611.004, of the Health and Safety Code. An important issue relates to the imminency of the client’s danger. Licensees should have adequate training to properly assess clients’ level of risk and when to involve law enforcement and/or medical personnel. Consultation with a supervisor or other licensee is also critical in proceeding with a possible imminent danger situation.
Many licensees may work for employers who have specific protocols that obligate the clinician to a higher standard than simply taking reasonable actions to inform others. For instance, LPCs working for an area mental health crisis center may be required to involve a psychitrist and arrange involuntary commitment of suicidal and homicidal clients.
Although Texas does not have a Tarsoff-like duty to warn third parties, one common approach is to notify law enforcement and or medical personnel of threats made by clients regarding specific individuals.
Protecting Clients in Therapy
681.41 (e) states that Texas LPCs must take reasonable precautions to protect their clients from physical or emotional har resulting from interaction with group or individual counseling. To protect clients from potential physical or emotional harm, LPCs implement a variety of reasonable precautions throughout the therapeutic process. First and foremost, they create a secure and confidential environment where clients feel safe to express themselves. This is often achieved through establishing clear boundaries, setting ground rules for interactions, and fostering a culture of respect and trust among participants. In group settings, LPCs carefully screen participants to ensure compatibility and minimize the risk of conflict or trauma triggers.
Moreover, Texas LPCs receive training in identifying and managing crises, which equips them to respond effectively if a client experiences extreme emotional distress during a session. They utilize techniques such as grounding exercises, de-escalation strategies, and active listening to support clients in navigating difficult emotions. Additionally, LPCs conduct thorough risk assessments and are attentive to any signs of potential emotional harm, such as anxiety or discomfort, thereby allowing them to intervene promptly if a therapeutic interaction becomes overwhelming.
LPCs are also guided by ethical standards and legal obligations that emphasize the importance of informed consent, ensuring clients fully understand the therapeutic process and any risks involved. They are trained to recognize and address power dynamics, especially in group therapy, where the interplay of different personalities can sometimes lead to vulnerability or intimidation. By prioritizing the mental and emotional safety of their clients, Texas LPCs not only maintain the integrity of the therapeutic relationship but also foster holistic healing and growth. Through ongoing professional development and supervision, LPCs continuously refine their skills and knowledge to further enhance the protective measures they employ, demonstrating a steadfast commitment to their clients' safety and welfare.
Rule 681.41 (f)
Texas Administrative Code §681.41(f) establishes a critical standard for mental health professionals, stipulating that a licensee must not evaluate an individual's mental, emotional, or behavioral condition unless they have personally interviewed the individual or disclosed that they have not conducted such an interview in their evaluation.
This regulation underscores the importance of interaction between the therapist and the client in the diagnostic process, which is essential for ensuring accurate assessments and ethical practice. The rationale behind this regulation is rooted in the necessity for accurate diagnosis and treatment in mental health care. Misdiagnosis can lead to inappropriate treatment plans that may exacerbate a client's condition rather than alleviate it.
Holowka et al. emphasize that diagnostic errors in mental health can result in inefficient treatment and significant harm to patients, highlighting the importance of thorough evaluations conducted through personal interviews Holowka et al. (2014). This aligns with the ethical standards that govern Texas LPCs, which mandate that practitioners engage directly with clients to gather comprehensive information about their conditions.
Moreover, the therapeutic alliance, which is crucial for effective therapy, is often built through personal interactions. Research indicates that a strong therapeutic alliance is associated with better treatment outcomes (Kramer & Stiles, 2015). When therapists bypass personal interviews, they risk undermining this alliance, which can lead to a lack of trust and engagement from the client.
The absence of a personal interview may also prevent therapists from picking up on non-verbal cues and other contextual factors that are vital for accurate diagnosis (Bernstein, 2023). The implications of failing to adhere to this regulation can be severe.
Therapists who do not comply with the requirement to personally interview clients may face disciplinary actions from regulatory bodies. Such actions could include revocation of licensure, fines, or mandated additional training, as these consequences serve to uphold the integrity of the mental health profession and protect clients from potential harm (Ahmed & Dennis, 2021). Furthermore, ethical violations related to inadequate evaluations can lead to legal repercussions, as clients may seek redress for harm caused by misdiagnosis or inappropriate treatment (Yang et al., 2010).
Texas Administrative Code §681.41(f) emphasizes the necessity of personal interviews in the evaluation of mental health conditions. This regulation is vital for ensuring accurate diagnoses, fostering therapeutic alliances, and maintaining ethical standards in practice. The potential consequences for failing to adhere to this standard highlight the importance of thorough and responsible clinical assessments in mental health care.
Rule 681.41 (g)
“A licensee must not knowlingly overtreat a client.”
Overtreatment occurs when a therapist provides more services than necessary, which can lead to financial, emotional, or psychological harm to the client.
Here are some examples of therapist overtreatment that could potentially violate this code:
1. Excessive Session Frequency: A therapist schedules clients for multiple sessions per week when bi-weekly or monthly sessions would have been sufficient based on the client's needs and treatment goals, leading to unwarranted financial burdens.
2. Recommending Unnecessary Assessments: A therapist may require clients to undergo extensive psychological testing or assessments that exceed what is clinically warranted, resulting in additional costs and stress for the client without contributing significantly to the treatment plan.
3. Unjustified Length of Treatment: Continuing therapy for an extended period without a valid clinical rationale, despite the client showing significant improvements or reaching their therapeutic goals, may be considered overtreatment.
4. Medical Treatment Referrals: A therapist might encourage clients to pursue numerous medical evaluations or procedures that are not substantiated by their symptoms or mental health issues, thus complicating their health care unnecessarily.
5. Excessive Homework: Assigning excessive amounts of therapeutic homework or tasks that overwhelm the client and distract from meaningful progress in therapy can also constitute overtreatment.
6. Group Therapy Overload: Encouraging clients to participate in multiple group therapy sessions in different settings simultaneously, leading to confusion and emotional fatigue rather than providing support.
7. Pressure to Attend Additional Services: A therapist may pressure a client into attending additional services, workshops, or supplementary therapy that is not aligned with their current treatment needs, primarily for monetary gain.
These examples illustrate how overtreatment can occur in therapeutic settings and underscore the importance of adhering to ethical guidelines to ensure client welfare and appropriate care. It's essential for therapists to evaluate their actions closely and seek supervision or consultation when unsure about the necessity of continued treatment.
Rule 681.41 (h) (i) and (j)
According to Rule 681.41 (h), LPCs in Texas have an obligation to uphold the integrity of their profession by not aiding or abetting anyone in practicing counseling without a proper license, as mandated by the law. This provision emphasizes the importance of maintaining professional standards and protecting the public by ensuring that only qualified individuals provide counseling services. Therefore, LPCs must remain vigilant against any unlicensed practices that could undermine the ethical and legal framework of the counseling profession.
Licensees must report to the Council any knowledge of non-licensed counseling practices. For instance, suppose that one of your co-workers is a Texas Licensed Chemical Dependency Counselor (LCDC) and does not hold any other licensure. LCDCs are not deemed qualified to treat individuals who are diagnosed with mental health disorders unless their presenting issues also include substance abuse or chemical dependency. This highlights the distinct roles within the counseling field, emphasizing that while LCDCs may address issues surrounding addiction, they should refer clients with primary mental health concerns to other qualified mental health professionals who possess the necessary training and expertise to offer comprehensive care in that domain. If such an individual were to engage in counseling beyond their scope, Rule 681.31 (i) requires it to be reported to the Council: “A licensee must report to the Council knowledge of any unlicensed practice of counseling.
Finally, paragraph (j) requires that licensees not participate in the falsification of any materials submitted to the Council. For example, any LPC-S providing supervision to LPC Associates are required to record accurate and precise supervision hours on the Supervised Experience Documentation Form. An over estimation of hours could be an example of submitting false information to the Council.
Rule 681.41 (k)
“A licensee must not provide services while impaired by a physical, mental, or medical condition or by medication, drugs, or alcohol.”
Counselor Impairment
• John is an LPC in private practice. He just returned to work after major surgery he underwent a week ago. His physician told him the surgery went well and John initially felt well enough to return to work. However, on his first day back, he began to experience some pain and didn’t think he could see a full caseload of clients, if any at all. He struggled throughout the day and decided to wait and see how the next few days went before reducing his schedule. John was under considerable stress to meet his financial obligations and knew any reduction in hours would be a hardship for him and his family.
• Talaia is a licensee going through a divorce. She has had many sleepless nights in recent weeks, but has not asked for any time off from her job as a counselor providing crisis counseling. Talaia has started to experience additional symptoms of depression in the last couple of weeks, but has not yet reached out for help. She is having more difficulty performing her duties as she once had. She appears preoccupied and is often tearful.
What is Impairment?
Some may hold a limited view of “impairment” that fails to consider scenarios like the ones of John and Talaia. Licensees may be tempted to restrict the definition to a co-worker struggling with alcoholism or drug addiction who shows up to work under the influence. Obvious intoxication may be the stereotypical definition of impairment, but encompasses a broader application of the term.
Rule 681.41 states that: “a licensee must not provide services while impaired by a physical, mental, or medical condition or by medication, drugs or alcohol.”
When is impairment determined for licensed counselors? At what point does behavior reach the threshold of poor insight and judgment that a licensee should postpone seeing clients? Impairment might involve any condition that prevents the licensee from acting in the best interests of their clients.
A general definition that might describe impairment as it applies to licensees is; “the inability of the counselor to provide professional services to the client, and/or uphold the responsibilities of a professional relationship with the client, and/or act in the best interests of the client.” Impairment is simply the inability to deliver competent patient care.
A counselor who is impaired has a greater likelihood of having lapses in judgment that may lead to improper advice, actions, or responses that harm the client. Impairment can come in varying degrees that is not always easy to assess; it is more concretely defined in some situations than others. For instance, a blood alcohol concentration of .08 or higher is considered too impaired to operate a motor vehicle. An employee who appears to be intoxicated at work can be taken for a drug screen. Such precise measures are not always available in determining a licensee’s impairment and if the licensee should delay work with clients.
Many of us can identify individuals impaired by alcohol, especially in the context of a party where alcohol is readily available. But other scenarios might be more subtle such as a licensee whose hangovers are interfering with job performance. A licensee who returns to work prematurely after surgery or illness and who is experiencing pain, could be experiencing some degree of impairment.
Complicated issues such as addiction, mental disorders, physical and health problems, burnout, family problems such as divorce or loss of a loved one, and many other issues, might impair a licensee’s ability to be professional with clients to one degree or another. The loss of a family member has the potential to render a licensee too impaired by grief to work with clients at least temporarily. Licensees must be diligent in recognizing their own vulnerabilities to many circumstances that impact their counseling skills.
The Blindside of Impairment
Impairment, as it is used in the two TAC rules that address it, involves a licensee’s lack of judgment and professional ability to work with clients. Impairment, by definition, might preclude a licensee from recognizing a need to address it. Asking an impaired person to rationally assess their impairment and take reasonable action to correct it would seem superfluous in many situations when impairment is severe. In these cases, a more direct and punitive intervention may be necessary when the licensee is unwilling or unable to cooperate.
Fortunately, there are many situations where impairment is not so severe that some degree of self-awareness and correction is possible. Also, it may be that family, friends, or co-workers can intervene before the worst is done. Licensees are encouraged to honestly look at, and prepare for, factors that could be impairing their judgement with clients now, as well as in the future.
The significance of an impairment may be minimized or overlooked because the impact of the condition or situation may not be obvious, or is suppressed through rationalization and denial; defense mechanisms common with some impairments. Even when impairment is obvious to the licensee or others, it may take a while before action is taken to address it.
A wedding reception or Super Bowl party, where a licensee may decide to consume more alcohol than usual, may require a plan in advance for additional time off. Some stressors require a licensee to make a judgement call about the degree of impairment it is creating and whether time off is required.
Medical emergencies, medication side-effects or adverse reactions, sudden tragic news, financial stress, childcare issues, family issues, and other aspects of life can create barriers to client care and may require time off from counseling obligations. A return to work too early for many different reasons is not an unrealistic danger.
Some impairments develop gradually. A licensee whose family problems starts out as something minor may gradually evolve into something that significantly distracts his focus away from optimum client care. The gradual nature of some impairments may blind us to its reality.
Many may have an intuitive understanding and ability to acknowledge when something is getting in the way of professional duties, but knowing at what point we can no longer serve clients effectively is not always clear.
Whether impairment can be anticipated or not, is gradual or arises suddenly, the ACA Code of Ethics advises that;
Counselors monitor themselves for signs of impairment from their own physical, mental, or emotional problems and refrain from offering or providing professional services when impaired. They seek assistance for problems that reach the level of professional impair- ment, and, if necessary, they limit, suspend, or terminate their professional responsibilities until it is determined that they may safely resume their work.
In the same section, counselors are charged with monitoring others in the field:
Counselors assist colleagues or supervisors in recognizing their own professional impairment and provide consultation and assistance when war- ranted with colleagues or supervisors showing signs of impairment and intervene as appropriate to prevent imminent harm to clients. (ACA C.2.g.)
Addressing Licensee Impairment
Prioritizing balance and self-care is important when thinking about protecting clients from harm. The well-being of licensees requires the professional to evaluate their professional and personal stressors, and address a re-balancing of personal priorities to establish order in their lives.46
Maintaining mental and physical stability are critical for counselors. Some helpful questions for licensees to resolve to prevent impairment might include:
• When was the last time I had a physical?
• Do I have at least one colleague with whom I can confide and who can be honest with me about my work with clients?
• Do I have any symptoms of alcoholism or drug abuse?
• Do I have any current symptoms of a mental, physical, or health related problem that could impair my abilities to work with clients in a professional relationship?
• Do I sometimes feel fatigued and overwhelmed when seeing clients?
• Do I exercise?
• Do I eat healthy?
• Do I have adequate family and social interactions, or do I smother myself in work?
These are only a few considerations in assessing one’s actual or potential for impairment. Any lapses in judgment have the potential to harm clients and could be the result of impairment.
RULE 681.42
Sexual Misconduct
Perhaps the most obvious and damaging form of boundary violation involves therapist/patient sexual and romantic relationships. Of all forms of boundary violations, many experts believe that these are the most harmful. At the time of this writing, 12% of the 235 pending complaints against Texas LPCs involved sexual misconduct.7
A number of studies have demonstrated that clients who are victims of therapist/patient sexual contact experience disproportionately high rates of adverse effects, including suicide. Experts also note that, perhaps to an even greater degree than other types of boundary violations, therapist/patient sexual contact is always, by definition, the therapist's fault.
In many jurisdictions, it is a criminal offense subject to a term of imprisonment; in all jurisdictions, it is a disciplinary offense and constitutes malpractice.
Sexual misconduct complaints receive the second highest priority of investigation by the BHEC behind cases involving probability of imminent physical harm to the public (TAC, 884.10). In one set of data of Texas LPCs, sexual misconduct violations were more common than violations related to confidentiality.
History
Concerns about sexual misconduct by health professionals are hardly new. The earliest published text to address the issue is the Corpus Hippocratum, "a body of about 70 medical texts compiled by the Library of Alexandria during the 4th and 5th centuries B.C." that includes the "Hippocratic Oath"8. The oath states, "I will abstain from all intentional wrong-doing and harm, especially from abusing the bodies of man or woman, bond or free" (Ibid). Others have found such admonitions as early as the code of the Nigerian healing arts9.
The founders of psychotherapy, including Freud, Jung, Breuer, and Ferenczi either engaged in or sanctioned sexual misconduct.10
Freud
Freud coined the term "transference" to describe the displaced feelings (including romantic and sexual feelings) that his patients developed for him during the analytical process. However, while he asserted that analysts should not become romantically or sexually involved with their patients, he excused such conduct by his male colleagues.
In the most glaring example, Freud inserted himself into a romantic relationship between one of his former students, Horace Frink, and one of Frink's patients. Freud not only urged Frink to leave his wife and marry the patient, but he evidently did so in the service of his own financial interests.11 The patient's family was wealthy, and Freud apparently believed that if Frink married the patient, her family would make a significant financial contribution to Freud's own work (Ibid).
Another incident involved Freud's former student, Ferenczi. One of Freud's former patients, Elma Pálos, later commenced therapy with Ferenczi; at the same time, her mother, Gisella Pálos, was romantically involved with Ferenczi and eventually would become his wife.12,13
However, while treating Elma, Ferenczi became sexually involved with her as well as with her mother (Ibid). While Freud had warned Ferenczi that he should avoid sexual activity with patients, with regard to his involvement with Elma and Giselle Pálos, he also reportedly tried "to influence [Ferenczi's] choice of a mate."14
Even in his criticisms of Ferenczi's sexual entanglements with patients, Freud appears to have dismissed such sexual contact as "old misdemeanors."15 For his part, Ferenczi contended that those "old misdemeanors," which he characterized as "[t]he sins of youth," "can make a man wiser... Now, I believe, I am capable of creating a mild, passion-free atmosphere, suitable for bringing forth even that which had been previously hidden".16
Carl Jung
Several years earlier, Carl Jung had likewise become sexually involved with a patient. Sabina Spielrein, a 19-year-old medical student in "desperate mental distress," first came to Jung for analysis and therapy in 1905 (Ibid, citing Gay, 1998). Jung treated her over the next four years, and, according to Gay, "[took] advantage of her dependency [and] made her his mistress" (Ibid).
However, Jung's exploitation of his young patient did not stop with the affair: Rumors of the affair began to circulate, and Jung assumed that Spielrein was responsible. He later admitted: "Caught in my delusion that I was the victim of the sexual wiles of my patient, I wrote to her mother that I was not the gratifier of her daughter's sexual desires but merely her doctor, and that she should free me from her."17
In that same letter, he justified shifting from a doctor/patient to a social relationship "the more easily" because he had not been charging Spielrein professional fees.18,19 He then suggested that if his patient wanted him "to adhere to strictly to [his] role as doctor," he was entitled to receive "a fee as suitable recompense for [his] trouble" (Ibid). As the situation worsened, Jung even asked Freud to intervene by writing to Spielrein's mother. Freud did so, and subsequently advised Jung not to blame himself for the mess, asserting, "[I]t was not your doing but hers" (Ibid).
Karen Horney
Women were not exclusively victims, however: Some of the early female professionals in the mental health field likewise engaged in sexual activity with patients. Karen Horney reportedly was involved in what she characterized as "restricted relationship[s]" with patients.20,21 Her biographer, Susan Quinn, describes a "romantic relationship" between Horney and a young male patient, which Quinn appears to rationalize as an example of "old impulsive ways [that] survived into middle age".22,23
Horney allegedly became sexually involved with patients and students with some regularity. Schoener describes Horney as having regularly "played favorites" with her lovers, temporarily elevating one to favored status, then suddenly replacing him with another.24,25
Incidence and Dynamics
It took a long time for the scope and even the existence of the problem to be acknowledged. In the late 1960s, the first research into the subject was undertaken, but the resulting report was suppressed by the Los Angeles APA, despite its own ethical prohibition against suppressing research findings.26
The earliest research into incidence rates for sexualized contact with health care providers came from a survey of psychiatrists, obstetrician/ gynecologists, surgeons, internists and general practitioners, and reported that as many as thirteen percent indicated that they had engaged in erotic behavior with clients, with 7.2% acknowledging sex.27
In the early 1970s, data from malpractice carriers and a poll of psychiatrists revealed that the problem was far more common than believed. In 1971, 11% of male psychiatrists admitted to having sex with at least one client. 80% of those psychiatrists had sex with multiple patients.28
It appears that the incidence rates of erotic contact between psychotherapists and their clients has decreased a great deal as a result of improved awareness of the issue, its consequences, and because of the large number of successful criminal prosecutions and civil suites, beginning with the 1968 case of Zipkin v. Freeman.
The legal bases for civic suits include negligence, malpractice and breach of fiduciary duty. Legislation was formulated beginning in 1983 that now includes criminal and civil statutes.29
The change in perception that began in the 1970s resulted in patients’ claims of sexual abuse by counselors and physicians to begin to be taken seriously. In the decades preceding this change, it was believed that such abuse was rare, that allegations were fantasies, and that allegations of incest were invalid for the same reasons. More time passed before there were laws and ethical codes addressing the problem.
It was not until 1991 that the American Medical Association’s Council on Ethics and Judicial Affairs codified the injunction against sex between physicians and their patients.30,31
Research
Recent research is not plentiful in the area of counselor sexual misconduct and its impact on clients. Prior research has associated the following problems resulting or being increased in clients by sex with their counselor: sexual dysfunction, anxiety disorders, psychiatric hospitalizations, suicide risk, depression, dissociative behavior, guilt, shame, anger, confusion, hatred, inability to trust and feelings of worthlessness.32 It has been estimated that only four to eight percent of victims ever report these experiences.33
McNulty34 conducted in-depth interviews with three individuals who had been found publicly in breach of standards of their professions due to sexual contact with clients or former clients. Due to the nature of such studies, it can be difficult to recruit study subjects and evaluation of the data is often a complex task. In this case, the researchers used interpretative phenomenological analysis (IPA) on the interview transcripts. This involves a systematic process of highlighting significant phrases and organizing the material into themes.35
A key theme found in the results was that all three individuals minimized the clients’ mental health problems. By minimizing the problems, boundaries appear to be dissolved. Two of the study subjects’ relationships occurred sometime after the end of the therapeutic relationship and even involved the couples becoming engaged. When the ex-clients’ mental health issues resurfaced and the relationships ended, this led to their reporting the relationship so that the therapists’ professional careers were ended.
Not surprisingly, the other theme found in this study involved the therapists being cast as hero in the initial stages, moving to a label of victim as the relationship unraveled.36 The authors interpreted their findings to indicate that the therapists employed strategies to equalize the relationship (by minimizing the mental health issues). Once the problems recurred, the relationship was not sustainable. It appears that clients suffer similar kinds of harm at similar rates regardless of the type of health care provider with whom they had sexualized contact.37
Although flaws have been pointed out, surveys of clients who have experienced sexual relationships with their counselors offer alarming numbers and types of harm. Even if one takes the position that this kind of harm is not typically the result of sex with a counselor, there remain the matters of abuse of power, the damage to the investment the client has made in counseling, the time and creative energies that the counselor has taken from the client, and the stresses and distractions posed by subjecting the client to circumstances that are highly socially stigmatized and humiliating.
In addition, from the perspective of society, there is the damage to the reputation of the profession of counseling, the effect this can have in reducing utilization of appropriate mental health services, and the resulting harm to citizens and society at large. The power imbalance between a psychotherapist and client brings into question the idea that there can be meaningful consent on the part of the client.38 In fact, Bitar recommend that therapists should soften the power differential with clients. They suggest that a more collaborative alliance will benefit the therapeutic process.39
Add to this the likelihood that a sexual relationship will cloud the judgment of the counselor, potentially resulting in harm or at least inadequate mental health care because of poor professional judgment.
It is very difficult to determine an accurate rate of occurrences of sex between counselors and clients. Early studies yielded numbers around 10% of psychiatrists and psychologists. Later studies showed the numbers dramatically declining. However, it is unknown whether the increased stigma and attention to the issue resulted in underreporting or an actual reduction in the rate.40 Sexual misconduct has resulted in a high percentage of malpractice suits against psychotherapists.41
The reason for clients not reporting sexual misconduct can be understood when one considers that lawsuits are often a matter of public record and may take many years to resolve.
Research on outcomes of treatment for counselors who sexually offend has not been encouraging, and these counselors have the ability to keep their sexual activities with their clients a secret for extended periods.
The topic of sexual misconduct has been studied in a variety of health care settings. Perhaps not surprisingly, there has been a spotlight on professions that – by definition – require the care giver to make physical contact with the client just to do their job. For example, in an online survey of 967 physical therapists, Roush42 explored the topic of sexual boundaries in a clinical setting. They found that most physical therapists comply with their profession’s Code of Ethics.
However, a number of respondents reported that they have dated current (1.0%) or former (9.5%) patients and condone patient “sexual banter” in the clinic. Close to half (42%) of the survey participants acknowledged having felt sexually attracted to a patient at some point.
When asked if they were aware of a colleague who dated former patients, more than half (51%) responded “yes.” Also, more than half (54%) of the survey respondents said they had been sexually propositioned or harassed by a patient.
More on RULE 681.42
Rule §681.42 of the Texas Administrative Code forbids licensees from engaging in "sexual contact" or "sexual exploitation" of any client, any LPC Associate supervised by the licensee, or a student at an educational institution at which the licensee provides professional or educational services. It also prohibits "therapeutic deception" of a client. These terms are defined below in the ensuing subsections. It also imposes reporting and other duties upon LPCs. These are also discussed below.
Irons defines professional sexual misconduct as “the overt or covert expression of erotic or romantic thoughts, feelings, or gestures by the professional toward the patient, that are sexual or may be reasonably construed by the patient as sexual.” This definition is consistent with that found in Rule §681.42, which addresses three specific types of sexual misconduct: "sexual contact"; "sexual exploitation"; and "therapeutic deception."
Sexual Contact
Under §681.42, "sexual contact" falls into four categories: The first three are "deviate sexual intercourse," "sexual contact," and "sexual intercourse” as defined by the Texas Penal Code, §21.01. The fourth category comprises "requests or offers by a licensee for conduct" that falls into one of the other three categories.
Texas Penal Code §21.01(1) defines "deviate sexual intercourse" as “any contact between any part of the genitals of one person and the mouth or anus of another person,” or “the penetration of the genitals or the anus of another person with an object.”
The Penal Code defines "sexual contact" as “any touching of the anus, breast, or any part of the genitals of another person with intent to arouse or gratify the sexual desire of any person.” The Code also defines sexual contact with a child as:
The following acts, if committed with the intent to arouse or gratify the sexual desire of any person:
(1) any touching by a person, including touching through clothing, with the anus, breast, or any part of the genitals of a child; or
(2) any touching of any part of the body of a child, including touching through clothing, with the anus, breast, or any part of the genitals of a person.
Finally, "sexual intercourse" is defined under the Texas Penal Code as “any penetration of the female sex organ by the male sex organ.”
Sexual Exploitation
§681.42 defines "sexual exploitation" as “a pattern, practice, or scheme of conduct, which may include sexual contact, that can reasonably be construed as being for the purposes of sexual arousal or gratification or sexual abuse of any person." Sexual exploitation thus includes much more than actual sexual contact. LPCs need to be aware that certain behaviors, comments, or gestures, however innocently intended, may be misinterpreted; particularly by patients who are unusually vulnerable with regard to such issues.
LPCs should also note the law's specific definitions of what may constitute sexual exploitation where the purpose is; "sexual arousal, gratification or sexual abuse of any person." Examples include:
(1) sexual harassment, sexual solicitation, physical advances, or verbal or nonverbal conduct that is sexual in nature, and:
(A) is offensive or creates a hostile environment, and the licensee knows, should know, or is told this; or
(B) is sufficiently severe or intense to be abusive to a reasonable person in the context;
(2) any behavior, gestures, or expressions which may reasonably be interpreted as seductive or sexual;
(3) sexual comments about or to a person, including making sexual comments about a person's body;
(4) making sexually demeaning comments about an individual's sexual orientation;
(5) making comments about potential sexual performance except when the comment is pertinent to the issue of sexual function or dysfunction in counseling;
(6) requesting details of sexual history or sexual likes and dislikes when not necessary for counseling of the individual;
(7) initiating conversation regarding the sexual problems, preferences, or fantasies of the licensee;
(8) kissing or fondling;
(9) making a request for a date;
(10) any other deliberate or repeated comments, gestures, or physical acts not constituting sexual intimacies but of a sexual nature;
(11) any bodily exposure of genitals, anus or breasts;
(12) encouraging another to masturbate in the presence of the licensee; or
(13) masturbation by the licensee when another is present.
Although 681.42 allows for sexual contact that occurs more than five years after the termination of the client relationship, cessation of supervision of an LPC Associate, or termination of professional or educational services provided to a student of the licensee at a post-secondary educational institution, there are stipulations. The conduct must be consensual, not the result of sexual exploitation, and not detrimental to the client.
The licensee must demonstrate there has been no exploitation in light of all relevant factors, including, but not limited to:
(A) the amount of time that has passed since therapy terminated;
(B) the nature and duration of the therapy;
(C) the circumstances of termination;
(D) the client's, LPC Associate's, or student's personal history;
(E) the client's, LPC Associate's, or student's current mental status;
(F) the likelihood of adverse impact on the client, LPC Associate, or student and
others; and
(G) any statements or actions made by the licensee during the course of therapy,
supervision, or educational services suggesting or inviting the possibility of a
post-termination sexual or romantic relationship with the client,
LPC Associate, or student.
The statute makes clear that "[t]he term ['sexual exploitation'] does not include obtaining information about a client’s sexual history within standard accepted practice while treating a sexual or marital dysfunction.”
However, LPCs must ensure that attempts to obtain such information are limited strictly to therapeutic purposes. Making such inquiries when they are not necessary to the therapeutic process may constitute sexual exploitation. Examples of such inquiries may include asking the patient for details of her sexual history, asking about sexual likes and dislikes, or making comments about potential sexual performance, when such questions or comments are not pertinent to the patient's course of treatment.
LPCs should also be aware that they may need to take special precautions in the area of self-disclosure. Self-disclosure is a valid therapeutic technique, used in various forms by many, if not most, therapists. However, clients who file complaints or lawsuits against LPCs frequently cite inappropriate or excessive self-disclosure as one of the bases of the complaint. According to Caudill:
Therapists must be conscious that excessive self-disclosure can fuel a patient's perception that he or she is special to the therapist, or that there is a potential for a relationship outside the therapeutic one. The problem becomes more acute when the patient is inquiring as to the therapist's personal life and/or the therapist’s relationships with his or her family and/or lovers. At that point, the therapist should be inquiring as to what purpose this information would serve for the patient to know (Caudill, 2000).
The LPC should engage in self-disclosure only when it is clearly for the client’s benefit. The client’s condition weighs upon this decision (Ibid).
Therapeutic Deception
A third category of sexual misconduct is "therapeutic deception." Rule 681.42 defines therapeutic deception as a representation by a licensee that sexual contact with, or sexual exploitation by, the licensee is consistent with, or a part of, a client’s or former client’s counseling." If an LPC encourages a client to engage in sexual contact by telling the client that such contact is part of her therapy, the LPC commits therapeutic deception and sexual exploitation.
The Code also forbids the defense that the sexual misconduct (sexual contact, sexual exploitation, or therapeutic deception) occurred: (1) with the consent of the client, LPC Associate, or student; (2) outside the professional counseling sessions of the client or student; or (3) off the premises regularly used by the licensee for the professional, supervisory, or educational services provided to the client, LPC Associate, or student.
For purposes of professional liability and the potential for disciplinary sanctions, the circumstances surrounding sexual misconduct conduct are irrelevant. This is true regardless of whether the conduct occurred outside the context of professional counseling sessions or off the LPC's professional premises, or even if the conduct was "consensual." Such conduct violates state law and the LPC Rules of Practice, and thus may subject the LPC to potential professional, civil, and even criminal penalties.
While LPCs’ compliance with state regulatory and ethical requirements may be motivated in part by the possibility of lawsuits and criminal penalties, ethical issues permeate the practice and process of counseling. Texas LPCs must have a clear understanding both of applicable rules and guidelines and of the extent to which personal experiences and biases may influence how they understand and apply these requirements.
Reporting
Under §681.42, if an LPC has reasonable cause to suspect that a client, LPC Associate, or student has been the victim of sexual exploitation, sexual contact, or therapeutic deception by another mental health provider, or if a client, LPC Associate, or student alleges such victimization by another licensee or mental health service provider, the LPC must report the alleged conduct not later than the third business day after the date the license became aware of the alleged conduct.
The report should be filed with the prosecuting attorney in the county in which the alleged sexual misconduct occurred, the BHEC (the Council), and any other state licensing agency which licenses the mental health provider if the conduct involves a licensed individual.
Before making the report, the LPC must inform the alleged victim of the LPC’s duty to report, and must determine whether the victim wishes to remain anonymous. The report must include the identity of the LPC making the report, identify the alleged victim unless the victim has requested anonymity, express suspicion that sexual misconduct occurred and provide the name of the alleged perpetrator.
ETHICS COMPLAINTS: The Process
Complaints are submitted to the BHEC on an approved form downloaded from their website. When a complaint is submitted to the BHEC, the person making the complaint waives the right to confidentiality. Complaints are required to be filed within five years of the complainant’s termination of services, but those alleging sexual misconduct are allowed to be filed within seven years after the date of termination or of the client turning 18, whichever is later.
BHEC refers cases to the Enforcement Division and gives priority to complaints in the following order:
• Cases involving a probability of imminent harm to the public or a member of the public;
• Cases involving sexual misconduct;
• Cases involving applicants for licensure; and
• Cases involving all other violations of state and federal law.
The following criteria are considered before proceeding:
• the allegations on their face state a violation of the law;
• the respondent is a licensee of the Council; and
• the activities or services involved are exempt from the Council’s jurisdiction.
If the criteria are met, the complaint is classified as a jurisdictional complaint, given a case number, and the licensee notified. The complaint proceeds forward in the Council’s investigatory process. If the criteria are not met the complainant is notified as to why the Enforcement Division could not investigate the complaint.
Probable cause means there is reason to believe a violation has occurred. If probable cause exists for the violation within the jurisdiction of the agency, the complaint proceeds possibly resulting in an agreed order or settlement offer. If the licensee rejects the proposed agreed order, the complaint is then set for an informal conference or, in cases requiring expert witnesses, a Disciplinary Review Panel.
If there can be no resolution to this point, the case will be referred to the State Office of Administrative Hearings (SOAH) and the case becomes a contested case. A contested case is similar to a bench trial where evidence, testimony of the complainant and licensee, and witnesses, can be presented before an administrative law judge. The judge will make a proposal for decision (PFD) with opinion as to whether a violation of law within the jurisdiction of the Council (BHEC) has occurred. The Council may then sanction the licensee or dismiss the complaint.
THE VOLUME OF COMPLAINTS AGAINST TEXAS LPCs
In the 3rd quarter of FY2022, there were a total of 235 pending complaints against Texas LPCs. In the same TSBEPC meeting minutes, it was recorded that 12 percent of pending allegations involved violations of Rule 681.42 (Sexual Misconduct). Of the complaints resolved in Q3, roughly 10 percent resulted in disciplinary actions. There were another 119 complaints that were dismissed during this same time period.
The majority of dismissed complaints were the result of “insufficient evidence,” but about 17% of these resulted in warning letters. The nature of these dismissed complaints involved issues regarding: Standard of Care, Unprofessional Conduct, Confidentiality, Record Keeping, Dual Relationship, Billing, Criminal History, Sexual Misconduct, and Fraud.
The sheer number of complaints indicate that allegations of ethics violations are not uncommon for Texas LPCs, but most do not result in disciplinary actions. Although the majority of complaints are dismissed, even those that are dismissed can be quite an emotional jolt and source of anxiety for licensees.
TIME INVOLVED WITH PROCESSING A COMPLAINT
Even complaints that do not result in disciplinary action can take considerable time. On average, complaints in the third quarter took well over a year to resolve, with only one-fourth being resolved in less than six months. Some allegations take several years to resolve. The BHEC states on their website; “The Council makes every effort to complete its investigations within 6 months, but the resolution of a complaint may take much longer.”
The BHEC has limited resources and must prioritize complaints. Complaints involving the probability of imminent danger to the public are given the highest priority followed by those involving sexual misconduct. All other complaints are investigated with less priority. Uncertainty of how long it will take for a complaint to be resolved is another reality of an alleged or actual ethics violation.
THE PENALTIES OF COMPLAINTS LEADING TO DISCIPLINARY ACTION
Individuals spend many years preparing to become licensed professional counselors. They can quickly jeopardize that privilege, temporarily or permanently, depending on the ethics infraction. There are a multitude of reasons for ethical failures ranging from careless oversight to outright criminal actions.
It is quite sobering to think of the potential consequences licensees incur from various violations. For complaints resulting in disciplinary action, the minimum penalty is often an administrative fine of a few hundred dollars. The maximum disciplinary sanction is revocation of the license, which may be accompanied by an administrative penalty of up to $5,000 per violation.
The severity of discipline depends on several factors including whether the case involved multiple violations or any aggravating or mitigating factors. Each violation constitutes a separate offense, even if arising out of a single act.
The Council may combine an administrative penalty with another standard disciplinary sanction. Punishment can come in three forms; 1) The loss of something (loss of license, license being restricted, etc.); 2) The requirement to do something (take additional continuing education, enter therapy, etc.), and/or; 3) a monetary fine. According to BHEC, the intent is “to protect the public or deter future violations.”
The meeting minutes of the TSBEPC contain on-going updates of disciplinary actions against licensees. A few Agreed Orders are included and provide some specificity regarding the penalties imposed by the Council.
In one case, an inappropriate and intimate relationship with the parent of a client led to the licensee resigning his license without the right to reapply for licensure for a minimum of ten years.
In another case, the Agreed Order stated a licensee failed to report suspected child abuse. This violation incurred a license reprimand, a fine of $1,000, and nine hours of professional development related to required reporting.
Other orders reflected various violations including failure to renew a license on time, failure to notify a client of termination and transfer to appropriate care, sexual exploitation, and failure to maintain confidentiality. Some of the penalties included loss of license, probated suspension, license reprimand, a fine of $2,000, required therapy for at least six months, and revocation of supervisor status.
In summary, complaints against licensees are not uncommon, take considerable time to resolve, and can result in significant penalties. This is not meant as a scare tactic, but rather a reminder of the reality of ethics violations and the consequences incurred when they can be substantiated. Often, an ethics violation can be avoided with simple reminders of the rules being enforced. Hopefully, courses like this one and others, can play some role in diminishing violations.
RULE 681.43 Testing
There is consensus within the counseling profession that testing is within the scope of practice of professional counselors. The American Counseling Association (ACA), The National Board for Certified Counselors (NBCC) and The American Mental Health Counseling Association (AMHCA) all recognize testing as part of counseling activities.43 The National Board of Certified Counselors Code of Ethics devotes no fewer than 15 paragraphs in its Directives section to the issue of tests and assessments.44
Other entities are congruent with the Texas Administrative Code in recognizing the role licensed professional counselors have in testing and assessment administration. In reference to the administration and interpretation of psychological tests, the National Board of Forensic Evaluators (NBFE) adopts the view that licensed professional counselors; “may administer and interpret such tests as long as they have received the appropriate training, and thus, are qualified to perform such procedures.”45
According to TAC 681.31 (Rules of Practice) and 681.43 (Testing), Texas LPCs with appropriate training, supervision, and experience can administer and interpret formal and informal instruments and procedures in individual and group settings for the purposes of determining a client’s strengths and weaknesses, mental status, emotional stability, intellectual ability, interests, aptitudes, achievement level and other characteristics for diagnosing mental health disorders.
Licensees are not permitted to diagnose a physical condition or disorder. Also, in accordance with the Texas Occupations Code 503.003(b)(1) LPCs are not allowed to use projective techniques. This includes instruments such as the Rorschach Inkblot Test, the Holtzman Inkblot Test, the Thematic Apperception Test, the Children’s Apperception Test, and the Senior Apperception Test.
Licenses, prior to or following the administration of any test, must make known to clients the purposes and explicit use to be made of the tests as a part of a professional counseling relationship. Licensees must not appropriate, reproduce, or modify copyrighted tests or any parts thereof without the acknowledgment and permission of the copyright owner.
Finally, licensees must observe the necessary precautions to maintain the security of any test they administer or the under the licensee’s supervision. As with any area of counseling, licensees should be appropriately qualified before administering tests.
RULE 681.44
NOTE: RULE 681.44 has been deleted as of LPC Rulebook dated March 24, 2025:
681.44 Drug and Alcohol Use. A licensee must not use alcohol or drugs in a manner that adversely affects the licensee’s ability to provide counseling.
A similar Rule remains:
Rule 681.41 (k): A licensee must not provide services while impaired by a physical, mental, or medical condition or by medication, drugs or alcohol.
Reasoned Justification (for repeal of 681.44).
The adopted repeal removes language identified during the quadrennial rule review as unnecessary and duplicative, without changing the substantive impact of the rules.
RULE 681.45 Confidentiality and Required Reporting
Confidentiality is fundamental to the counselor-client relationship. Without it, the public would not trust therapists to guard sensitive information, and would not have the openness that is necessary for effective counseling. Clients desire privacy for many reasons, especially their concern about social stigma. Confidentiality helps to protect the dignity of individuals and prevents sensitive information from falling into the wrong hands and being used against clients.
Even the appearance of impropriety regarding confidentiality may threaten public perception regarding psychotherapy. Therefore, licensees should not discuss clients publicly, even when they feel they are disguising enough details to preserve confidentiality. This is especially important online or in public presentations. Ethical guidelines, as well as state and federal law, protect the confidentiality of medical records.
Even when an authoritative-sounding person demands information about a client, licensees do not reveal whether the individual is their client without clear legal permission and knowledge that it is in the client’s best interest.
Licensees should have the following response ready: “I can neither confirm nor deny that this individual is or has ever been my client.” Even if the information has become public knowledge, the therapist is still under the duty to protect privacy.
CONFIDENTIALITY OF INFORMATION AND PROHIBITION AGAINST DISCLOSURE.
According to TAC 681.45 (a), Communication between a licensee and client and the client's records, however created or stored, are confidential under the provisions of the Texas Health and Safety Code Chapter 611 and other state or federal statutes or rules where such statutes or rules apply to a licensee's practice.
Paragraph (b) of 681.45 states that a licensee must not disclose any communication, record, or identity of a client except as provided in Texas Health and Safety Code Chapter 611 or other state or federal statutes or rules unless it is authorized in the Health and Safety Code.
Exceptions to Confidentiality
Texas law is very similar to other states regarding exceptions to confidentiality. It includes exceptions such as organizations involved in paying the client’s fees, and guardians of persons adjudicated as incompetent. This is in section 611.004 of the Health and Safety Code, Title 7, subtitle E, Special Provisions Relating to Mental Illness and Mental Retardation. It is worth reproducing here because it is very specific and concise:
(1) to a governmental agency if the disclosure is required or authorized by law;
(2) to medical or law enforcement personnel if the professional determines that there is a probability of imminent physical injury by the patient to the patient or others or there is a probability of immediate mental or emotional injury to the patient;
(3) to qualified personnel for management audits, financial audits, program evaluations, or research, in accordance with Subsection (b);
(4) to a person who has the written consent of the patient, or a parent if the patient is a minor, or a guardian if the patient has been adjudicated as incompetent to manage the patient's personal affairs;
(5) to the patient's personal representative if the patient is deceased;
(6) to individuals, corporations, or governmental agencies involved in paying or collecting fees for mental or emotional health services provided by a professional;
(7) to other professionals and personnel under the professionals' direction who participate in the diagnosis, evaluation, or treatment of the patient;
(8) in an official legislative inquiry relating to a state hospital or state school as provided by Subsection (c);
(9) to designated persons or personnel of a correctional facility in which a person is detained if the disclosure is for the sole purpose of providing treatment and health care to the person in custody;
(10) to an employee or agent of the professional who requires mental health care information to provide mental health care services or in complying with statutory, licensing, or accreditation requirements, if the professional has taken appropriate action to ensure that the employee or agent:
(A) will not use or disclose the information for any other purposes; and
(B) will take appropriate steps to protect the information; or
(11) to satisfy a request for medical records of a deceased or incompetent person pursuant to Section 74.051(e), Civil Practice and Remedies Code.
(b) Personnel who receive confidential information under Subsection (a)(3) may not directly or indirectly identify or otherwise disclose the identity of a patient in a report or in any other manner.
(c) The exception in Subsection (a)(8) applies only to records created by the state hospital or state school or by the employees of the hospital or school. Information or records that identify a patient may be released only with the patient's proper consent.
(d) A person who receives information from confidential communications or records may not disclose the information except to the extent that disclosure is consistent with the authorized purposes for which the person first obtained the information. This subsection does not apply to a person listed in Subsection (a)(4) or (a)(5) who is acting on the patient's behalf.
Revocation of Release of Information
Section 611.007 of Health and Safety Code Subtitle E addresses revocation of release of information. At any time after a client has given permission to disclose information to someone, the client can revoke that release. However, “A revocation is valid only if it is written, dated, and signed by the patient or legally authorized representative.”
The client cannot “revoke a disclosure that is required for purposes of making payment to the professional for mental health care services provided to the patient.”
The text referenced above regarding fee-paying organizations bears a resemblance to HIPAA language that allows an informed consent form to establish that certain routine communications can take place without specifying the recipient in writing. However, unlike HIPAA, Texas law does not say that licensees establish such an informed consent condition for disclosures to other professionals involved in the client’s treatment, or to close family members concerned with the client’s welfare. Barring case law or competent legal advice to the contrary, the law is best interpreted as requiring a specific signed release of information. It states that the LPC “may disclose confidential information...to a person who has the written consent of the patient...” in its list of exclusive permissions.
The only other mention of clinicians in these sections are specialized, and would not cover treating clinicians in general. HIPAA law does not trump state law where it is less restrictive or specific. It is designed to allow states to set up additional requirements as they see fit.
Section 181 of the Health and Safety Code covers “Consumer Access to Electronic Health Records.” It indicates that a provider that uses electronic records must (when not excepted) provide requested records within 15 business days of receipt of written request, and shall provide them in electronic form unless the person agrees to another form. It also spells out serious financial penalties for breaches of privacy for electronic health records, ranging from $5,000 to $250,000 per violation, depending on factors such as intentionality, any pattern of recidivism, and the size of the business
Reporting Abuse, Exploitation and Neglect
As in all states, mental health professionals have a duty to report suspected abuse, neglect, or exploitation of children, the elderly, or dependent adults. They also must make a report to protect the health and safety of a child or dependent adult when their primary information is that an adult has been abused by someone. This situation would arise, for example, if the person suspected of abuse is now a caretaker for or cohabiting with a child and allegedly abuse the adult when the adult was a child.
Reports are to be made immediately to the Department of Family and Protective Services; Child Welfare and Protective Services.
ATTENTION: UPDATE on Change in Mandatory Reporting Deadline for Suspected Child Abuse from TEXAS BHEC received on 7/16/2025:
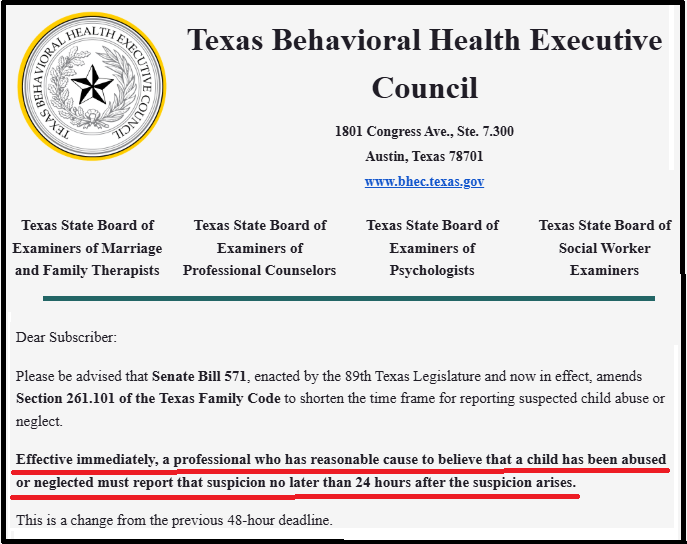
The report must contain the following information:
(1) the name, age, and address of the elderly or disabled person;
(2) the name and address of any person responsible for the elderly or disabled person's care;
(3) the nature and extent of the elderly or disabled person's condition;
(4) the basis of the reporter's knowledge; and
(5) any other relevant information.
The law on child abuse reporting is in Family code, Title 5, Subtitle E, Chapter 261, “Investigation of Report of child Abuse or Neglect, Subchapter B. Report of Abuse or Neglect; Immunities.
The law on the elderly and dependent adults is in Human Resources Code, Title 2, Subtitle D, chapter 48, Investigations and Protective Services for Elderly and Disabled Persons, Subchapter B, Reports of Abuse, Neglect, or Exploitation; Immunities, Sec. 48.051, Report.
The Right to the Mental Health Record
Texas and federal law indicate that clients have a right to their mental health record. Subtitle E, Section 611.0045 covers this right and its exceptions.
The law gives the conditions under which the record (or a portion of it) may be denied to the client, and it indicates the responsibilities associated with such a denial. This, again, is very specific and concise, so it is reproduced below. The law is very similar to that of other states.
Note:
(a) Except as otherwise provided by this section, a patient is entitled to have access to the content of a confidential record made about the patient.
(b) The professional may deny access to any portion of a record if the professional determines that release of that portion would be harmful to the patient's physical, mental, or emotional health.
(c) If the professional denies access to any portion of a record, the professional shall give the patient a signed and dated written statement that having access to the record would be harmful to the patient's physical, mental, or emotional health and shall include a copy of the written statement in the patient's records. The statement must specify the portion of the record to which access is denied, the reason for denial, and the duration of the denial.
(d) The professional who denies access to a portion of a record under this section shall redetermine the necessity for the denial at each time a request for the denied portion is made. If the professional again denies access, the professional shall notify the patient of the denial and document the denial as prescribed by Subsection (c).
(e) If a professional denies access to a portion of a confidential record, the professional shall allow examination and copying of the record by another professional if the patient selects the professional to treat the patient for the same or a related condition as the professional denying access.
(f) The content of a confidential record shall be made available to a person listed by Section 611.004(a)(4) or (5) who is acting on the patient's behalf.
(g) A professional shall delete confidential information about another person who has not consented to the release, but may not delete information relating to the patient that another person has provided, the identity of the person responsible for that information, or the identity of any person who provided information that resulted in the patient's commitment.
(h) If a summary or narrative of a confidential record is requested by the patient or other person requesting release under this section, the professional shall prepare the summary or narrative.
(i) The professional or other entity that has possession or control of the record shall grant access to any portion of the record to which access is not specifically denied under this section within a reasonable time and may charge a reasonable fee.
(j) Notwithstanding Section 159.002, Occupations Code, this section applies to the release of a confidential record created or maintained by a professional, including a physician, that relates to the diagnosis, evaluation, or treatment of a mental or emotional condition or disorder, including alcoholism or drug addiction.
(k) The denial of a patient's access to any portion of a record by the professional or other entity that has possession or control of the record suspends, until the release of that portion of the record, the running of an applicable statute of limitations on a cause of action in which evidence relevant to the cause of action is in that portion of the record.
Privilege
A privilege is a legal rule that protects communications within certain relationships from compelled disclosure in a court proceeding. It is the legal term for the licensee’s obligation to preserve the privacy of clients. Privilege is a legal concept normally dictated by rules of evidence.
Section 611.003 of the Health and Safety Code states that the privilege of confidentiality may be claimed by the licensee, but only on behalf of the client. And, the authority of a professional to claim the privilege of confidentiality on behalf of the patient is presumed in the absence of evidence to the contrary.
Privilege is understood to address a conflict between two obligations. For example, if a counselor receives a subpoena to release clinical records, he or she must “assert the privilege,” that is, assert to the court that the client’s right to privacy is a greater mandate than the subpoena. Licensees should consult with an attorney in such cases.
RULE 681.46
Licensees and the Council
Licensees are required to adhere to the regulations set forth in the Act and related chapters, as well as the rules established by the Council. This legal framework ensures that licensees maintain a high standard of practice within their profession. Additionally, it is the responsibility of each licensee to report any suspected violations of the Act or the relevant chapters to the Council. This obligation is crucial for upholding the integrity of the regulatory system and ensuring accountability among all licensed professionals. By fulfilling this duty, licensees contribute to the overall enforcement of the law and the protection of public interest.
RULE 681.47
NOTE: In LPC Rulebook dated March 24, 2025, Rule 681.47 regarding Assumed Names has been deleted:
681.47. Assumed Names.
(a) An individual practice by a licensee may be established as a corporation, a limited liability partnership, a limited liabiliy company, or other business entity in accordance with state or federal law.
(b) An assumed or trade name used by a licensee must not be false, deceptive, or misleading as those terms are described in 681.49(b) of this title (relating to Advertising and Announcements).
The Texas Behavioral Health Executive Council on behalf of the Texas State Board of Examiners of Professional Counselors adopts the repeal of §681.47, relating to Assumed Names.
Reasoned Justification:
The adopted repeal removes language identified during the quadrennial rule review as potentially in conflict with the Texas Business and Commerce Code, while not changing the substantive requirement in other rules that a licensee not make or benefit from false, misleading, deceptive, fraudulent, or exaggerated claims.
RULE 681.49
NOTE: In LPC Rulebook dated March 24, 2025, only paragraph (8) of Rule 681.49 regarding Advertising and Announcements has been deleted:
[(8) makes a representation that is designed to take advantage of the fears or emotions of a particularly susceptible type of patient; or]
Reasoned Justification.
The adopted amendments remove language identified during the quadrennial rule review as potentially unenforceable, while not changing the substantive requirement that a licensee not make or benefit from false, misleading, or deceptive advertising
The remaining Rule on Advertising and Announcements remains unaltered.
Advertising and Announcements
In addition to therapists being aware of avoiding misleading statements to clients about their qualifications or making promises about treatment outcomes, therapists need to be equally mindful about any statements made in advertisements or marketing materials. Rule 681.49 sets out specific requirements for Advertising and Announcements.
The rule essentially prohibits statements that are false or misleading – see the first section here:
Section 681.49 - Advertising and Announcements
(a) Information used by a licensee in any advertisement or announcement must not contain information which is false, inaccurate, misleading, incomplete, out of context, deceptive or not readily verifiable.
It’s important to note that the rule does not just cover advertising but also “announcements;” that term applies to most other written statements from one’s business, such as brochures, letterhead, and even billing statements.
It’s useful to give separate consideration to formal advertising language and then to how a practice is presented on printed materials such as letterhead. We’ll discuss each of those requirements.
Advertising
False advertising in the counseling profession can lead to serious ethical dilemmas and potential legal repercussions for practitioners. One notable example is that of a therapist who promoted themselves as a "life coach" and claimed to possess qualifications and success records that were either exaggerated or completely fabricated. This individual marketed specialized programs that promised rapid transformations, but clients quickly realized that the methods employed were not backed by any credible psychological principles. As a result, clients began filing complaints, and regulatory bodies investigated the claims, ultimately leading to the revocation of the individual’s license to practice.
Another instance occurred when a counseling center advertised their services as "guaranteed healing" for a range of mental health conditions, including depression and anxiety. The center utilized testimonials from clients without their consent and presented anecdotal evidence as factual results. This misrepresentation not only misled potential clients but also attracted the attention of consumer protection agencies, which scrutinized their advertising practices. Following an inquiry, the center faced significant fines and was required to alter its marketing strategies to adhere to ethical guidelines.
These examples underscore the importance of integrity and honesty in the counseling profession. Misleading advertisements not only undermine public trust but also can lead to a cycle of harm for vulnerable clients seeking genuine support. The consequences of false advertising are a stark reminder for counselors to adhere to ethical standards and promote their services truthfully, prioritizing the welfare of those they serve above all else.
Blatant lies by therapists are not the norm when it comes to advertising. The more common issue pertains to advertising that may be misleading. Generally, in the counseling sphere, the standard is whether the consumer could be misinformed.
The rule sets out nine types of actions to avoid. The first two cover generally false and misleading statements generally, and a prohibition against unjustified claims about outcomes:
(b) False, misleading, or deceptive advertising or advertising that is not readily subject to verification includes advertising that:
(1) makes any misrepresentation of fact or omits a fact necessary to make the statement misleading;
(2) makes any representation likely to create an unjustified expectation about the results of a mental health care service or procedure;
Many experts recommend that therapists ask a trusted colleague to review advertising statements with an eye towards anything that might mislead a potential client. Three areas to focus on are what a therapist says about services offered, testimonials, and expertise.
Services Offered
One current issue over description of services involves use of the term evidence-based therapy.
This term is commonly referenced term in advertising today. In at least one case, a complaint has been filed with a state board indicating the term is misleading customers.
A therapist in one state asked the licensing board to caution practitioners that claims about evidence-based therapy often display a misunderstanding of the term and confuse potential clients:
“Many in the field of psychotherapy, including practitioners and marketing personnel, are currently using the term “evidence-based therapy” to refer to something quite different from what someone might otherwise assume. It is, therefore, misleading and problematic. I am requesting this board to treat such incorrect and misleading claims as false advertising.”50
The complaint goes on to explain that empirically supported treatments (ESTs) have been demonstrated to be effective in controlled clinical trials, but evidence-based therapy entails a broader range of clinical activities as defined by the American Psychological Association.
The concerns raised are that consumers will confuse clients in several ways. First, promoting an approach as evidence-based when it really isn’t is misleading on its face. Second, the term itself can lead consumers to believe that other therapy modes are less legitimate.
Ultimately, she argues this type of advertising in effect limits the choices for a consumer trying to decide what’s best for them. A compelling argument, since the standard is whether the advertising would misinform a potential client.
In today’s social media climate, therapists need to be cautioned that a Facebook page promoting one’s practice is considered advertising. If the page is set up to market a counseling service, then all statements need to conform with the advertising ethical standards.
The Texas Rule 681.49 (b)(3) also warns again comparing one’s services with another health care professional's services “unless the comparison can be factually substantiated.”
Testimonials
Therapists also must use caution with any client testimonials used. Rule 681.49 (b)(4) prohibits any “…testimonial that includes false, deceptive, or misleading statements, or fails to include disclaimers or warnings as to the credentials of the person making the testimonial.”
On this subject, the American Counseling Association has clarified that reviews and sometimes even a “like” on social media pages can be considered testimonials. The ACA prohibits counselors from soliciting testimonials, but it’s becoming common in social media for consumers to offer reviews.
Therapists are reminded to consider the effect on the client, and educate the client on the risks and benefits of doing so. One risk being that the client is giving up their confidentiality; the benefit would be if they truly want to help others as they have been helped. Licensees should consider the client’s presenting issue and treatment progress, as to whether a public statement would be in the client’s best interests at that time.51
The ACA article clarifies that a client “liking” a Facebook page could be considered a testimonial. They recommend that practitioners develop a social media policy as part of their practice management, to show they are aware of these issues and are monitoring them.
Expertise and credentials
Counselors also need to pay attention to the details of how they describe their expertise – this includes claiming to have any specialties, and also the labelling of one’s credentials. Rule 681.49 (b)(5) states that advertising can be false and misleading if it “causes confusion or misunderstanding as to the credentials, education, or licensure of a mental health care professional.”
It's important to read the details of the rule on this topic. For example, a counselor can list their highest degree earned in counseling, or a counseling-related field, and also degrees in other areas provided the subject of the degree is specified (681.49 (d) & (e)). One’s licensing stature must be properly stated:
…”by the use of a title such as "Licensed Counselor", or "Licensed Professional Counselor", or "LPC", or a statement such as "licensed by the Texas Behavioral Executive Council" with reference to the "Texas State Board of Examiners of Professional Counselors." (681.49 (g)).
An LPC Associate must indicate their “Associate” status on all advertisements (681.49 (h)). Council-approved supervisors can use the designation "LPC-S" in their announcements (681.49 (j)).
Counselors must be careful if they claim any specialties. For example, Rule 681.49 (i) clarifies that a therapist might use art therapy as a counseling method, but if they don’t have the official art therapy specialty designation, they cannot advertise as an "art therapist" or use the initials "AT."
Announcements Including Letterhead, Business cards, etc.
Rule 681.49 also applies to “any announcement of services, letterhead, business cards, commercial products, and billing statements.” So counselors need to keep this in mind with regard to any depiction of credentials or services in print, or online. All of the above rules apply to how a counselor lists their title, degrees, services, etc., in any publication.
Statements made about health insurance coverage also need to be reviewed carefully. Consumers might be confused about whether services are fully covered by insurance or if deductibles or co-payments apply. These two rules clarify that a statement about insurance coverage can be misleading if it:
• advertises or represents that health care insurance deductibles or co-payments may be waived or are not applicable to health care services to be provided if the deductibles or co-payments are required; (681.49 (b)(6))
• advertises or represents that the benefits of a health benefit plan will be accepted as full payment when deductibles or co-payments are required; (681.49 (b)(7)).
Finally, the rule clarifies that if a therapist hires a third party for advertising or marketing, the therapist remains responsible for following ethical requirements (681.49(c)).
The Impact of Remote Counseling
It is no secret that companies advertising their counseling services, especially online services, has become pervasive in recent years. Celebrities have partnered with large mental health platforms to diminish the stigma associated with therapy and persuade viewers to use specific online counseling providers.52
Some believe the new tech companies offering remote counseling are threatening traditional brick-and-mortar practices, as well as how licensees are paid. These companies could potentially change the traditional private practice model, in the same way Uber impacted the private taxi industry. 53
The opposition to remote counseling is well documented. One argument is that the nature of the counseling relationship requires face to face interaction; that telehealth prevents the counselor-client relationship from developing its necessary components.
Regardless of one’s position regarding the pros and cons of online counseling, the COVID-19 pandemic forced more clients to be seen remotely. The residual effect has been to strengthen the argument for, and acceptance of, remote therapy. 54
Some companies employing licensees spend millions of dollars in advertising each month hoping to secure clients.55 The voluminous employment ads from these companies seeking licensed professionals is evidence of a growing online counseling industry.
The exact amount of dollars shifting from brick-and-mortar counseling to remote, online services, is difficult to know. The impact of competition and the degree to which a particular licensee will need to rely on advertising to generate leads in the future, is uncertain.
Whether a licensee offers remote services or not, there is often a need to have some sort of presence online even if only a simple website that provides basic information about the licensee’s background and population served. Some licensees may expend almost no effort in establishing lines of referral to stay in business, while others may have to depend heavily on advertising as a way to generate leads.
Now, with greater competition from large conglomerates with deep pockets, licensees may have to be more assiduous in allotting and spending advertising dollars effectively if they hope to flourish in private practice. Advertising must be creative enough to invite the interests of potential clients while upholding the TAC rules that govern it.
Texas LPCs who advertise their services are required to follow the guidelines in TAC Chapter 681. In addition to Rule 681.41 that restricts false or misleading statements from being made about a licensee’s qualifications or treatment outcomes in any context, Rule 681.49 specifies many similar requirements associated specifically with Advertising and Announcements.
The pressure to secure clients can be a reality in many areas of counseling, especially in the private sector. Some counselors in private practice thrive, while others find it difficult to maintain anything close to a full-time caseload. Administrators in private hospitals may understand the importance of effective advertising in building a consistently higher census.
Many licensees familiar with the promotion of a private practice understand how easily money can be wasted when advertising dollars are spent carelessly. If advertising does not result in clients, it is probably not wise to continue that advertising campaign.
RULE 681.50
Research and Publications
In conducting research involving human participants, a licensee holds the responsibility of ensuring the emotional and physical safety of those involved, taking reasonable precautions to prevent any potential harm. Furthermore, protecting the identity of clients is paramount; any data sourced from professional counseling relationships must be handled with the utmost confidentiality, particularly when utilized for educational or research purposes. Additionally, when engaging in research or disseminating findings, a licensee is obligated to acknowledge prior works in the field and adhere strictly to copyright regulations. Lastly, it is essential for licensees to accurately credit individuals who have made significant contributions to their research or publications, utilizing methods such as joint authorship, acknowledgments, or footnotes to give rightful recognition. These principles underpin ethical standards in research, fostering a respectful and responsible approach to the study of human experiences.
RULES 681.51, 681.52 and 681.53 are not addressed in this course.

Conclusion
Many of the standards mentioned in this course can be summed up by Rule 681.38(a): “A licensee must not engage in activities for the licensee's personal gain at the expense of a client.”
The first part of this course emphasized the importance of LPCs being trained appropriately in any method or technique they use with clients. The importance of using evidence-based practices, as well as the challenges in doing so, were discussed.
The accuracy and truthfulness of statements to clients about a licensee’s credentials, as well as the claims about the benefits of counseling, were emphasized. Next, the requirements of a professional relationship were explored including the elements of informed consent and limits on confidentiality.
This course expounded on the issue of non-therapeutic relationships; defined in the TAC as any non-counseling activity initiated by either the client or counselor resulting in a relationship unrelated to therapy. The guidelines for relationships, including sexual contact, with former clients was provided. Also, the definition of sexual misconduct, its definition, and the process of required reporting it, was explained.
The topic of concurrent counseling, where a client sees two licensees at the same time, was reported on. The process of a complaint made against a licensee was provided based on BHEC guidelines.
Rule 681.43 regarding Testing; Rule 681.44 on Drug and Alcohol Use; Rule 681.45 on Confidentiality and Required Reporting; Rule 681.49 regarding Advertising and Announcements were examined.
All of these guidelines intend to provide as much protection as possible to the needs of the clients we serve. The protection of the public is one of the most important functions of the BHEC and TSBEPC. This course is meant to remind Texas LPCs of the special influence and responsibilities we have been charged to keep with those under our care.
Licensees are reminded of the overall mission of the Texas State Board of Examiners of Professional Counselors; “The Board’s mission is to protect the people of Texas by ensuring professional counselors are qualified and competent practitioners. The board establishes qualifications for licensure, as well as the ethical standards to practice as a professional counselor in the state of Texas.”
According to the BEHC website, the primary responsibility of a regulatory body is to protect the interests of the public and not to advocate for the profession or its members. The Council works to ensure that the services provided by its licensees are ethical, competent, and consistent with acceptable standards.
References furnished upon request